Learning objectives
|
Introduction
Approximately 30% of all stroke patients suffer from post-stroke visual impairment. Hemianopia is the most common symptom, but also neglect, diplopia, reduced visual acuity, ptosis, anisocoria, and nystagmus are frequent. Homonymous hemianopia is seen in about 8% of those who have had a stroke, some of whom are still driving [1].
Aetiology
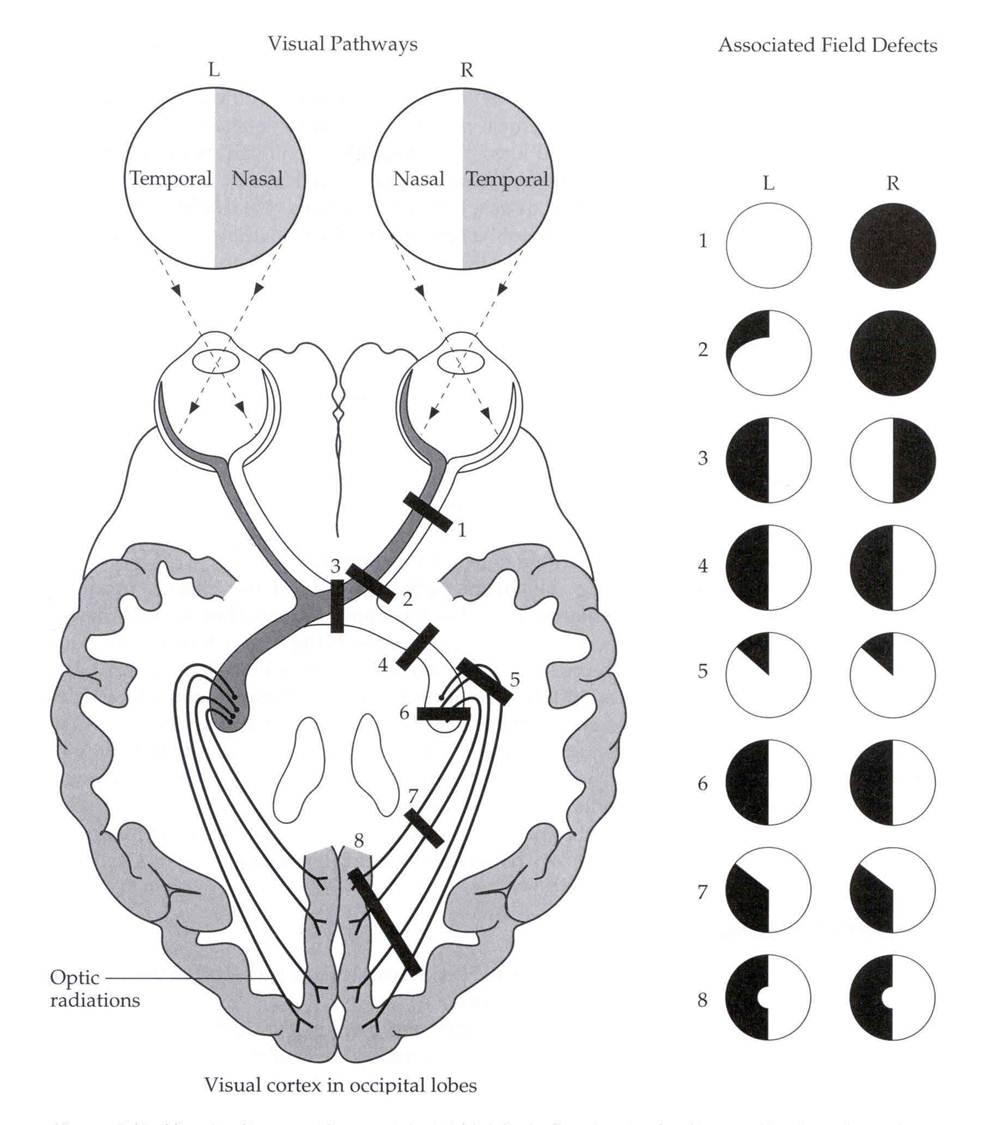
Homonymous hemianopia is a loss of the same (homo) right or left halves (hemianopia) of the visual field of both eyes. It usually occurs as a result of a middle cerebral or posterior cerebral artery stroke affecting either the optic radiation or visual cortex of the occipital lobe or haemorrhage in the temporal/parietal or occipital lobe. AN important fact is that the tip of the occipital lobe may receive a dual blood supply from both the PCA and end arteries of the MCA and thus the central or macular portion of the visual field of the patient may not be affected, resulting in an HH with macular sparing. Less severe and debilitating effects may be seen with quadrantanopia such as a superior quadrantanopia due to damage to the optic radiation inferiorly in the temporal lobe or an inferior quadrantanopia is caused by damage to the parietal lobe optic radiation.
Range of Field losses
| Visual Loss | Cause and summary |
|---|---|
| Altitudinal field defect | Loss of all or part of the superior or inferior half of the visual field; does not cross the horizontal median may be BRAO, Ischaemic optic neuropathy, retinal detachment, glaucoma |
| Central scotoma | Patch of visual loss. Macular disease, optic neuropathy/atrophy |
| Monocular (blind in one eye) | Can be due to localised eye disease from the cornea to the optic chiasma. Al patients need an Ophthalmological assessment. It may be vascular due to central retinal artery occlusion. Determine if artertitic (GCA) or non arteritis (embolism) by looking for a history of GCA/PMR, age and looking for vascular risk factors. May image ipsilateral carotid. |
| Monocular quadrantanopia, altitudinal Retinal defects | Can be due to localised eye disease and such as Branch retinal artery occlusion |
| Dynamic moving loss one or both eyes perhaps scotoma, bright rim, fortification spectra | Migraine with aura |
| Bitemporal hemianopia defects | Usually due to a pituitary tumour or craniopharygioma in a child. Needs Pituitary MRI with contrast |
| Lower homonymous quadrantanopia | Contralateral Temporal lobe pathology |
| Upper homonymous quadrantanopia | Contralateral Parietal lobe pathology |
| Complete homonymous hemianopia + sensory/Motor symptoms or signs | Large Parietal/Temporal lobe stroke usually MCA |
| Complete homonymous hemianopia no sensory/motor symptoms or signs | Large Occipital lobe stroke usually PCA |
| Complete blindness | Rarely stroke unless multiple simultaneous lesions |
| Prosopagnosia | Unable to recognise faces |
Left Homonymous hemianopia from patient's perspective

Visual Neglect
This a form of spatial inattention to one side of the body. Seen with dominant parietal lobe lesions. It can occur with or without a homonymous visual field defect. It may prove difficult for the person to compensate because they cannot mentally attend to that side. A man may only shave one side of his face. A patient will describe a well-known image and fail to mention the things to their left side. It provides challenges for recovery and these patients usually benefit from occupational therapy to learn to attend the affected side. There may be associated with abnormal eye movements as there are frontal and parietal eye fields that help initiate and modulate a saccade movement to initiate look to one side and maintain the gaze at a position. There may be impaired fast eye movements to the side of impaired vision which contribute to reading difficulties
Hemianopic alexia
This is a specific patterns of reading deficit caused by a focal brain lesion, usually a stroke, often affecting the left hemisphere. Reading involves using the righthand side of a word to help plan reading eye movements across the line of the text. A right HH and resulting hemianopic alexia results in deficiencies in this process with insufficient eye movements and text reading. Reading impairment poststroke is commonly reported and can be severely debilitating.
Driving
There is a significant effect of a complete hemianopia on a person's peripheral vision and driving. Patients may pose a risk to themselves and the general public if they have a poststroke visual field defect and continue to drive. It is important that all stroke physicians, nurses and therapists are aware of the current guidelines regarding fitness to drive. All those who drive and have experienced visual loss must be advised not to drive until a full assessment has been done. They may need formal assessment to check they pass the DVLA requirements
Minimum standards for field of vision - all drivers
The minimum field of vision for Group 1 driving is defined in the legislation:[3]
- A field of at least 120° on the horizontal measured using a target equivalent to the white Goldmann III4e settings.
- The extension should be at least 50° left and right. In addition, there should be no significant defect in the binocular field that encroaches within 20° of the fixation above or below the horizontal meridian.
- This means that homonymous or bitemporal defects that come close to fixation, whether hemianopic or quadrantanopic, are not usually acceptable for driving.
If the DVLA needs a visual field assessment for determining fitness to drive, it:
- requires the method to be a binocular Esterman field test
- may request monocular full field charts in specific conditions
- exceptionally, may consider a Goldmann perimetry assessment carried out to strict criteria
The Secretary of State's Honorary Medical Advisory Panel for Visual Disorders and Driving advises that, for an Esterman binocular chart to be considered reliable for licensing, the false-positive score must be no more than 20%. When assessing monocular charts and Goldmann perimetry, fixation accuracy will also be considered.
Management
- Team approach to educate, and identify risks and use of aids and other techniques to manage
- Useful information sheet for Patients
- Ophthalmologists, orthoptists, doctors and occupational therapists can advise on the best management for you.
- Prognosis is difficult to predict and a wait and see approach is wise.
- I tend to wait 2-3 months and then review formal field tests.
- Prism lenses can be used to shift images from the non-seeing to the seeing visual field.
References
- [1] Gilhotra JS, Mitchell P, Healey PR, et al. Homonymous visual field defects and stroke in an older population. Stroke 2002;33:2417-20.
- [2] Visual field defects after stroke. Reprinted from Australian Family Physician Vol. 39, no. 7, July 2010 499
- [3] DVLA Minimum standards for field of vision - all drivers Last updated 31 August 2018