Introduction
It is important to develop your ability to study imaging and correlate it with brain structure and function. There is a standard anatomical vocabulary with terms such as axial, sagittal and coronal which are commonly used in both CT and MR to describe different cross sectional images. Modern day imaging actually allows the brain to be imaged and reconstructed in any plane but these are the standard and familiar views.
Look at as much brain imaging as possible, the ones
that you request and more. The key is to see a wide variety of
normality and to build up some pattern matching skills and experience
in identifying important structures and lesions. You will have an
advantage over the radiologist who has only the clinical details on the
card whereas you have the patient.
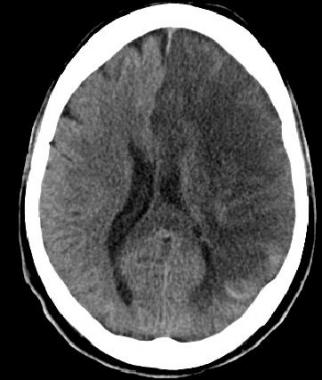
CT Interpretation
Definitive distinctive changes may not occur until 6-8 hours. In the meantime more subtle signs are seen. At about 6 hours and sometimes earlier there may be loss of grey-white matter differentiation - seen at the cortical surface due to localised changes such as cytotoxic oedema within the grey matter which has a higher metabolic requirement and so becomes oedematous quicker. These signs are subtle and can be missed by even the most experienced
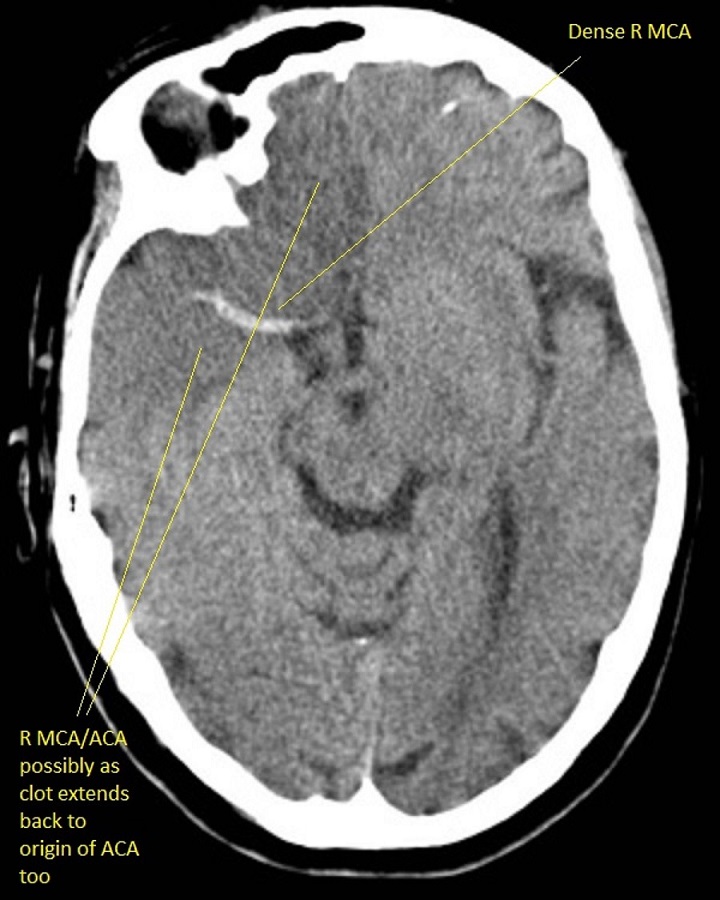
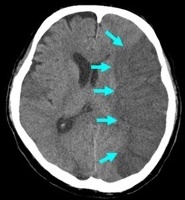
Left MCA hyperdense artery
This can be the earliest sign of a large vessel stroke if accompanied by a corresponding Left MCA stroke syndrome. There are no obvious tissue changes and the patient if within the window and NIHSS is raised and no contraindications should be considered for thrombolysis / thrombectomy if safe. Occasionally due to good collaterals theremay be minimal symptoms and in others they can be profound. A dense artery may just be calcium in the vessel wall and scans must be interpreted within the clinical context.

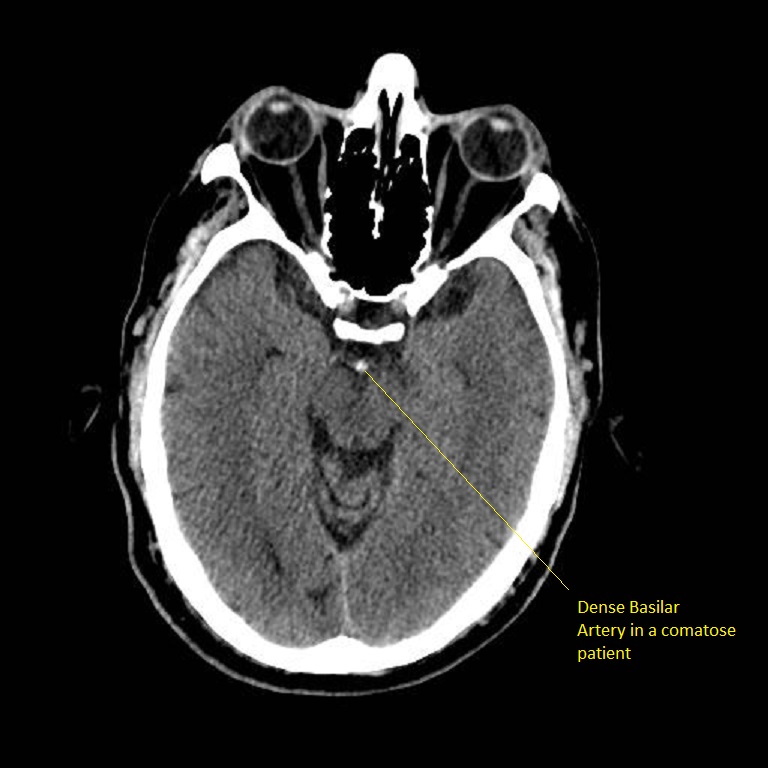
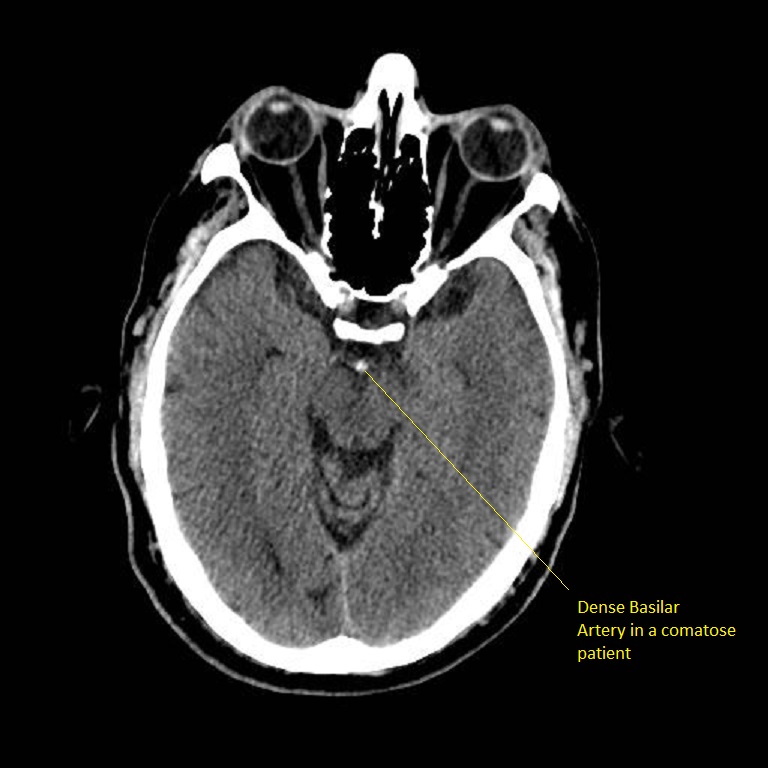
Dense Basilar Artery
The patient was comatose and sustained massive damage to the posterior circulation. This is an important sign in a deteriorating and comatose and quadriplegic patient needing consideration for thrombectomy. There are no parenchymal changes seen yet.
Early signs : less than 6 hrs of Acute Ischaemic Stroke
- May be entirely normal initially
- Cortical Sulcal effacement - suggests some increased oedema
- Loss of Grey/White differentiation in the basal ganglia
- Loss of insular ribbon sign is similar to loss of grey white differentiation with localised cytotoxic oedema. Vascular supply here is more vulnerable due to poor collateralisation and so this may show first.
- Obscuration of the Sylvian fissure: Similar to insular ribbon sign
- Hypoattenuation seen on CT is highly specific for irreversible ischaemic brain damage and infarction if it is detected within first 6 hours.
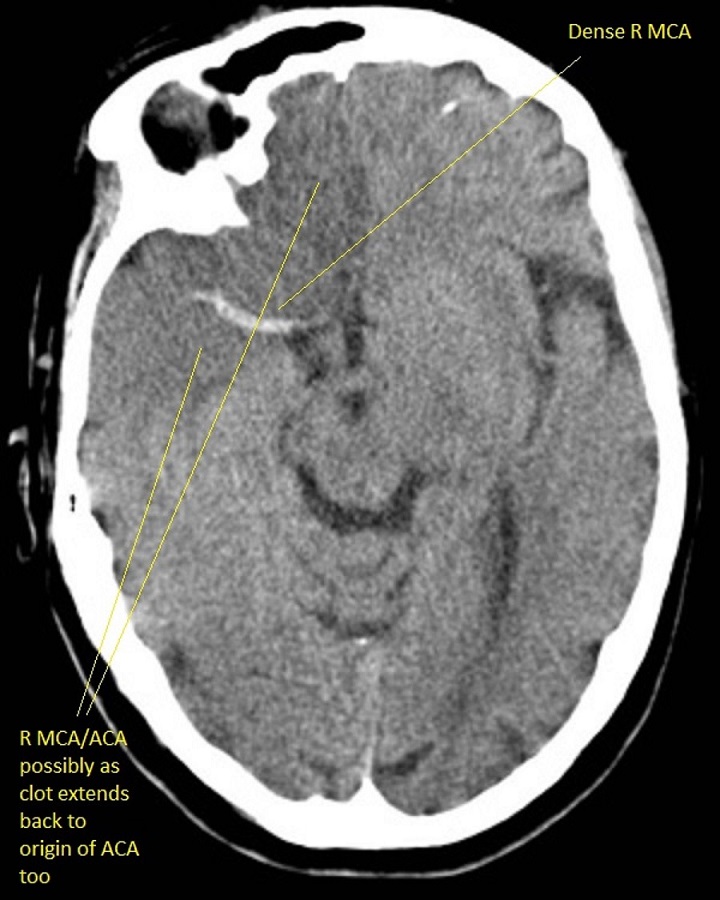
- Hyperdense MCA sign or more distal MCA "dot sign" it may be normal is a sign of clot (thrombotic or embolic) (not a contraindication to lysis) but shows extent of possible infarct which depends also on collateral flow.
- Obscuration of the lentiform nucleus (loss of the normal attenuation difference of the globus pallidus and/or putamen with respect to contiguous white matter structures
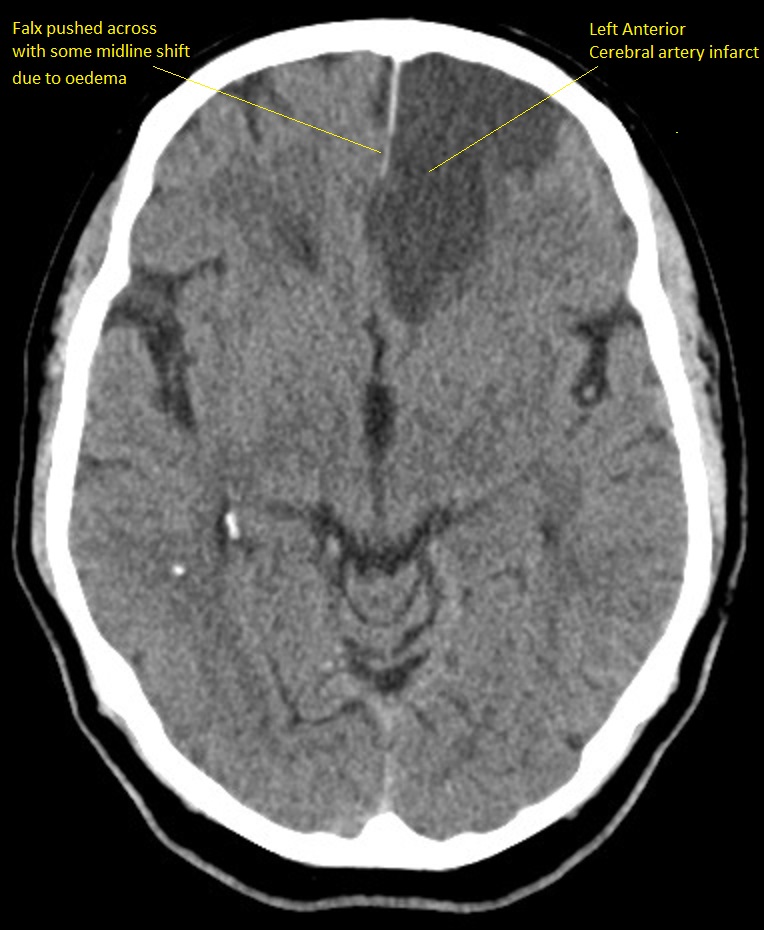
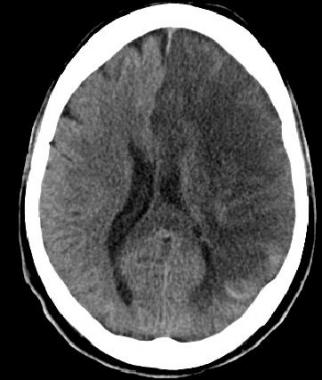
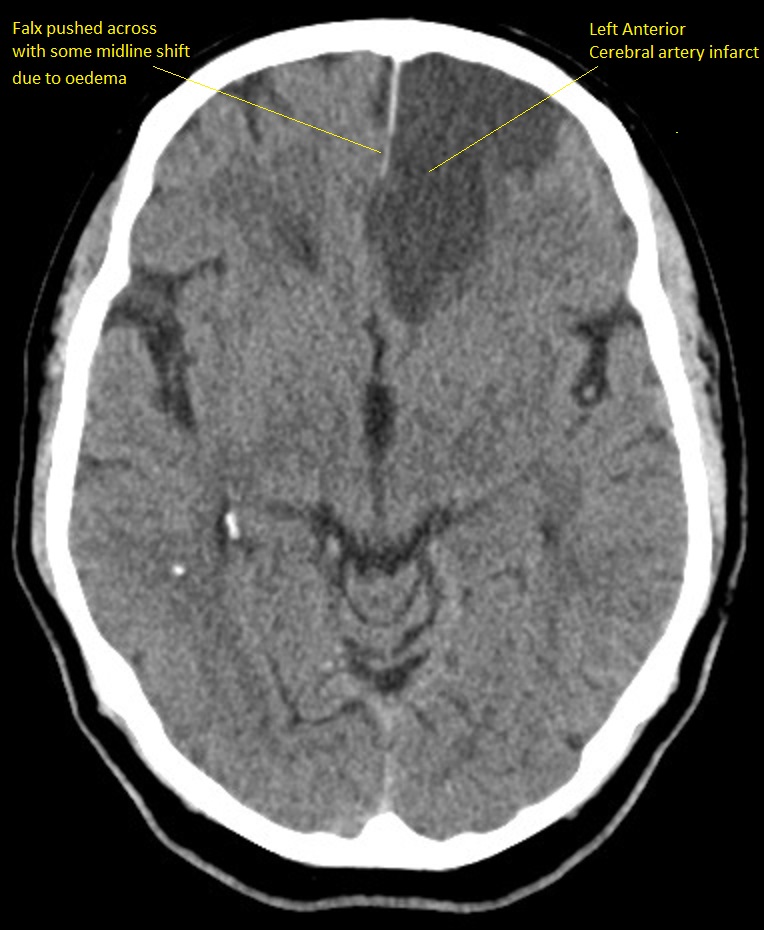
Developed Anterior Cerebral Artery Infarct
This shows an evolved subacute infarct as the edges are still indistinct and so there is ongoing liquefactive necrosis. This is about Day 2-4 or beyond. There is some mild midline shift due to some localised oedema.
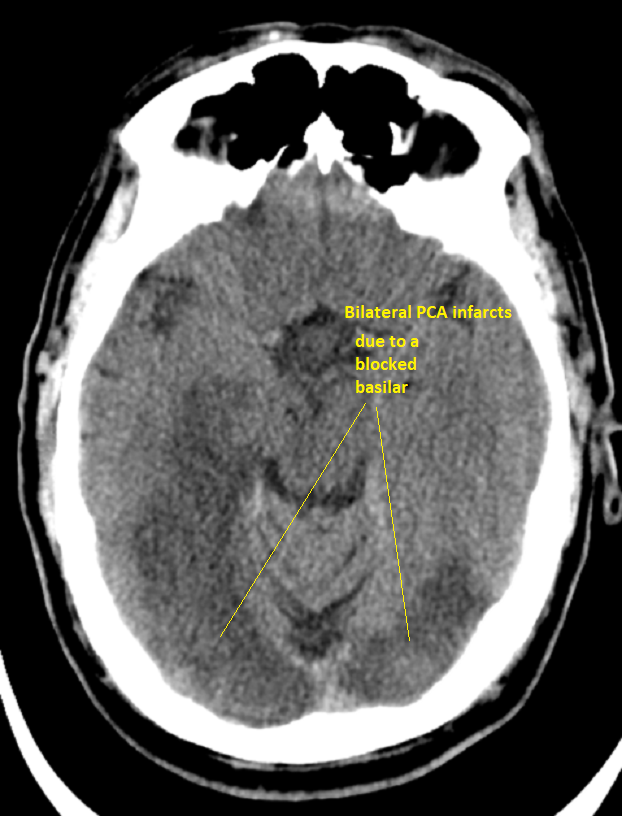
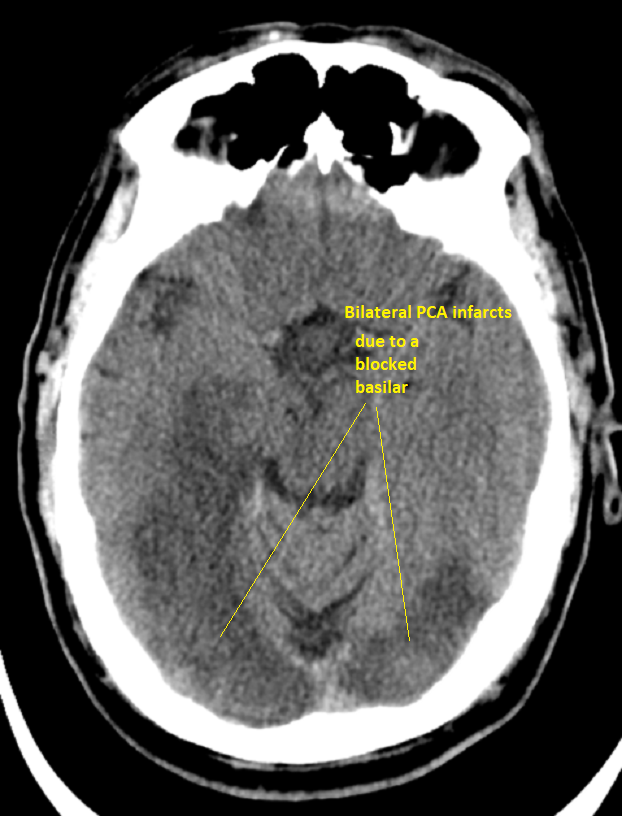
Bilateral PCA infarcts due to Basilar occlusion seen above
Infarction involves both occipital lobes. The patient who survived is blind.
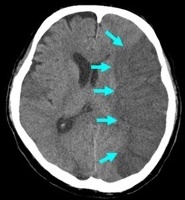
Large left Subdural Haematoma
There is no bright white fresh blood so this is a subacute bleed and it can be surprising how well these are tolerated. The midline is shifted. This is not stroke. It needs urgent discussion with neurosurgeons. Any anticoagulants or antithrombotic therapy must be stopped. The decision on whether to operate will depend as well on the clinical state of the patient.

| Later signs (6-24 hrs) of Acute Ischaemic Stroke |
|---|
- Watershed infarcts between vascular territories often bilateral strokes between ACA and MCA territory and MCA and PCA may suggest carotid disease
- Clearly delineated wedge shaped hypodense region involving cortex and adjacent white matter related to the occluded artery anatomy and collaterals at 12 hours.
- May be some haemorrhagic transformation. Estimated incidence of haemorrhagic transformation is up to 40% in the subacute period even when not thrombolysed.
- Lacunar infarcts may be seen deep within white matter and within the basal ganglia.
- Occasionally due to collateralisation or perhaps reperfusion of the MCA the cortex remains unaffected but subcortical areas infarct
and become hypodense and this is seen with a subcortical striato-capsular type of stroke.
- Late changes over days and weeks is most marked Hypodensity due to cytotoxic oedema initially and Vasogenic oedema secondarily and best seen days 3-10.
|
|
| Late signs ( > 24 hrs) of Acute Ischaemic Stroke |
|---|
- Fogging - density of ischaemic tissue reaches same intensity as normal brain tissue and so evidence of infarction not seen
- Late changes over weeks and months shows continue as the infarcted zone has density of CSF and there is loss of volume.
- A hypodense caudate suggests MCA occlusion proximally taking out lenticulostriate arteries.
- Depends on leptomeningeal anastomoses of ACA and PCA
- Haemorrhagic transformation may occur
|
|
Non contrast CT false negatives (there is a stroke) usually in infarcts when
done early or in those who present 7-10 days after stroke and there is
a visible hypodensity but no blood and so aetiology of perhaps a small
bleed may be missed. In these cases a gradient echo will show
haemosiderin deposition around the margins suggesting haemorrhage as he
cause.
NCCT false positives are seen particular in older hypertensive
patients where Lacunar infarcts are common and most often asymptomatic
but appear on scans done for a myriad of reasons so unless there is
corresponding new neurology do not diagnose acute stroke but do treat
for "stroke disease".