Learning objectives
- Learning
- Understand
- Integrate
- Reflect
|
Introduction
- Hereditary haemorrhagic telangiectasia (HHT), also known as Osler-Weber-Rendu disease
- Rare autosomal dominant genetic disorder that leads to abnormal blood vessel formation
- Telangiectasia found in the skin, mucous membranes
- Others found in the lungs, liver, and brain
- Most Cerebral AVMs in the HHT population are symptomatic.
- Family history of a parent, sibling or child with same
| The prevalence of brain AVMs in HHT patients was 10.4% in a large analysis of trials with no significant difference between males and females |
Aetiology
- A disorder of angiogenesis with abnormal fragile blood vessels
- Mutations in several genes, including the ACVRL1, ENG, and SMAD4 genes
- HHT1 patients more likely to have brain AVMs than HHT2 patients.
Aetiology of stroke
- Bleeding from a cerebral vascular malformations
- Paradoxical embolism through a pulmonary AVM (rare)
- The vessels lack contractile elements and so given direct arterial connection, bleeding from telangiectases can be brisk and difficult to stop. This may be seen with GI Bleeds.
| Most individuals with a PAVM(s) have Hereditary haemorrhagic telangiectasia |
Clinical
- Difficulties with Epistaxis seen in most by adulthood
- GI bleeding, Haematemesis, Melaena, Fe deficiency anaemia often over age of 50
- Haemorrhagic stroke as risk of AVMS
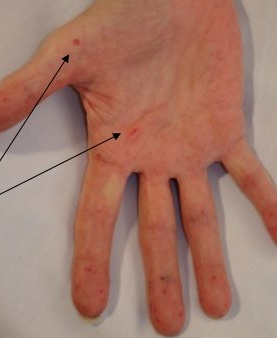
- Mucocutaenous lesions in skin and oral cavity and nose
- Embolic stroke via paradoxical embolism via pulmonary AVM
- Pulmonary AVM can rupture, leading to haemoptysis
Clinical Signs
Types
- Type 1: mutations in the ENG gene. Brain AVMS in 13.4 %
- Type 2: mutations in the ACVRL1 gene. Brain AVMS in 2.4 %
- Juvenile polyposis/hereditary haemorrhagic telangiectasia syndrome is caused by mutations in the SMAD4 gene.
Differential
- Vasculitis rash
- Thrombocytopenia
- Telangiectases of chronic liver disease are spider like with a central core and small vessels radiating outward
Diagnostic clinical criteria
| Diagnostic clinical criteria |
|---|
- Epistaxis (nosebleeds): spontaneous and recurrent.
- Mucocutaneous telangiectases: multiple, at characteristic sites (lips, oral cavity, fingers, and nose). Lesions are blanchable and usually punctuate, pink-red in color, and pinpoint to pinhead in size. Occasionally 2–5 mm macules,
purple or “spidery.”
- Vascular
- Visceral AVM.
- Pulmonary
- Cerebral
- Hepatic
- GI
- Spinal
- Family history: a first-degree relative in whom HHT has
been diagnosed using these criteria.
The clinical diagnosis of HHT is considered:
- Definite when three or more findings are present;
- Possible or suspected when two findings are present; and
- Unlikely when fewer than two findings are present.
Note: These diagnostic criteria were established for adults
and can be misleading when applied to children.
|
Investigations
- FBC: exclude Fe deficiency anaemia from GI blood loss. ESR, CRP, U&E, LFTs
- Brain Imaging - CT/MRI
- CXR : may show lung lesion ? AVM
- Angiography is AVM suspected. The Spetzler-Martin grade for HHT related lesions is 2 or less in nearly 90% of patients.
- Bubble echo shown to be a sensitive screen for PAVMs and then CT Pulmonary angiogram if positive bubble echo. This avoids radiation in young adults. This may need repeated at 5 year intervals.
- Colonoscopy and upper endoscopy +/- capsule endoscopy. Those with mutations in the SMAD4 gene may be at increased risk for polyps. Alternatively may be done to exclude other cause of Fe deficiency anaemia
- Molecular genetic testing is used to establish the genetic subtype of hereditary haemorrhagic telangiectasia in a clinically affected individual and family, and for early diagnosis to allow for appropriate screening and preventive treatment.
Management
- ABC, Stroke management, Acute management for GI Bleed as needed. Transfusion if needed.
- ENT referral for epistaxis - Laser ablation is usually recommended as the intervention for control of mild to moderate nosebleeds
- Gastroenterology review for GI bleeds. Iron replacement therapy for anaemia.
- Avoid antithrombotic drugs. Antifibrinolytic drugs such as tranexamic acid have been used in select patients
- Genetic counselling.
- Management of Cerebral Arteriovenous Malformations if found. A recent study has found that functional outcomes were not statistically different between those who had surgery and those who didn't on long term follow-up. Link
- Closure of Pulmonary AVM if embolic stroke by Interventional neuroradiology if needed.Any PAVM with a feeding artery > 1–3 mm detected by chest CT should be considered for treatment by transcatheter embolization.
References