Introduction
Epidemiology is defined in wikipedia as the study and analysis of the distribution and determinants of health and disease conditions in defined populations. With respect to stroke it helps to show the number of new strokes per year (incidence)and the numbers of those living who have had a stroke (prevalence). We can also see the effects of stroke in terms of mortality. The distribution of stroke in a population can also help us to highlight potential causes and relationships. Finally it helps us to plan and invest in and deliver appropriate hospital and community services.
Impact
Stroke is the third biggest killer in England and Worldwide and is the main cause of adult neurological disability - Stroke killed more than 40,000
people in 2009 in England and over 12,000 in NHS Midlands and East. Stroke is common, dangerous and expensive and for many is either lethal or disabling. In the UK it is the third biggest killer after heart disease and cancer . It is the main cause of adult disability. Stroke killed more than 40,000 people in 2009 in England and over 12,000 in NHS Midlands and East. Stroke causes chronic disability, is the second leading cause of dementia. Acute ischaemic stroke accounts for 85% of all strokes whilst the remaining 15% is attributable to haemorrhage. The last two decades have seen major advances in the diagnosis and management of stroke. This has resulted in a significant decline in the age standardized incidence, mortality and disability adjusted life years between 1990 and 2013. Despite this the burden of stroke rises as the mean age of the population rises and because of the growth of populations. Demand for stroke services will only continue to rise. Older patients are more likely to have an increased risk of frailty and multiple co-morbidities, and are
also more likely to have a severe stroke, which makes their care and management more complex and more costly.
Around two thirds of people will survive their stroke, but half of stroke survivors are left with long term disability and dependent on
others for everyday activities. There are an estimated 900 000 stroke survivors in England, half of whom are dependent on others for care at
an estimated cost of £8bn per year (about €9bn or $13bn for our overseas readers). Over 300,000 people are living with moderate to severe disabilities as a result of stroke. The direct cost of stroke to the NHS is estimated to be £2.8 billion. The cost to the wider economy is £1.8 billion. The informal care cost is £2.4 billion. Stroke patients occupy around 20 per cent of all acute hospital beds and 25 per cent of long term beds. Stroke units save lives: for stroke patients general wards have a 14% to 25% higher mortality rate than stroke units.
In a study across Europe total stroke incidence ranged in men ranged from 101.2 to 239.3 per 100000 (95% CI,82.5 to 123.0). The risk of stroke among European populations in our study varied more than 2-fold in men and women. On average, higher rates of stroke were observed in eastern and lower rates in southern European countries. The annual incidence of TIA is around 0.05% of the population of the UK. The good news is that stroke incidence rates fell 19% from 1990 to 2010 in the UK. The average age of stroke affected patients has decreased in recent years.
Facts and Figures
| For every 100,000 people in a year in the UK there are |
|---|
| Incidence is 164 First Strokes + 57 Recurrent Strokes |
| 10 Subarachnoid haemorrhages |
| 44 Male stroke Deaths |
| 33 Female Stroke Deaths |
| Prevalence 1,500 existing stroke cases |
| Prevalence 1,000 with moderate disability following stroke |
Stroke risks
- Age: Risk doubles for every successive decade after the age of 55 years
- Sex: 24% to 30% higher in men; however, absolute annual number of women experiencing stroke is higher because women outlive men
Race ethnicity
- 2- to 4-fold higher among African Americans and occur at an earlier agea
- 2-fold higher among Hispanics and occur at an earlier agea
- Higher among Chinese
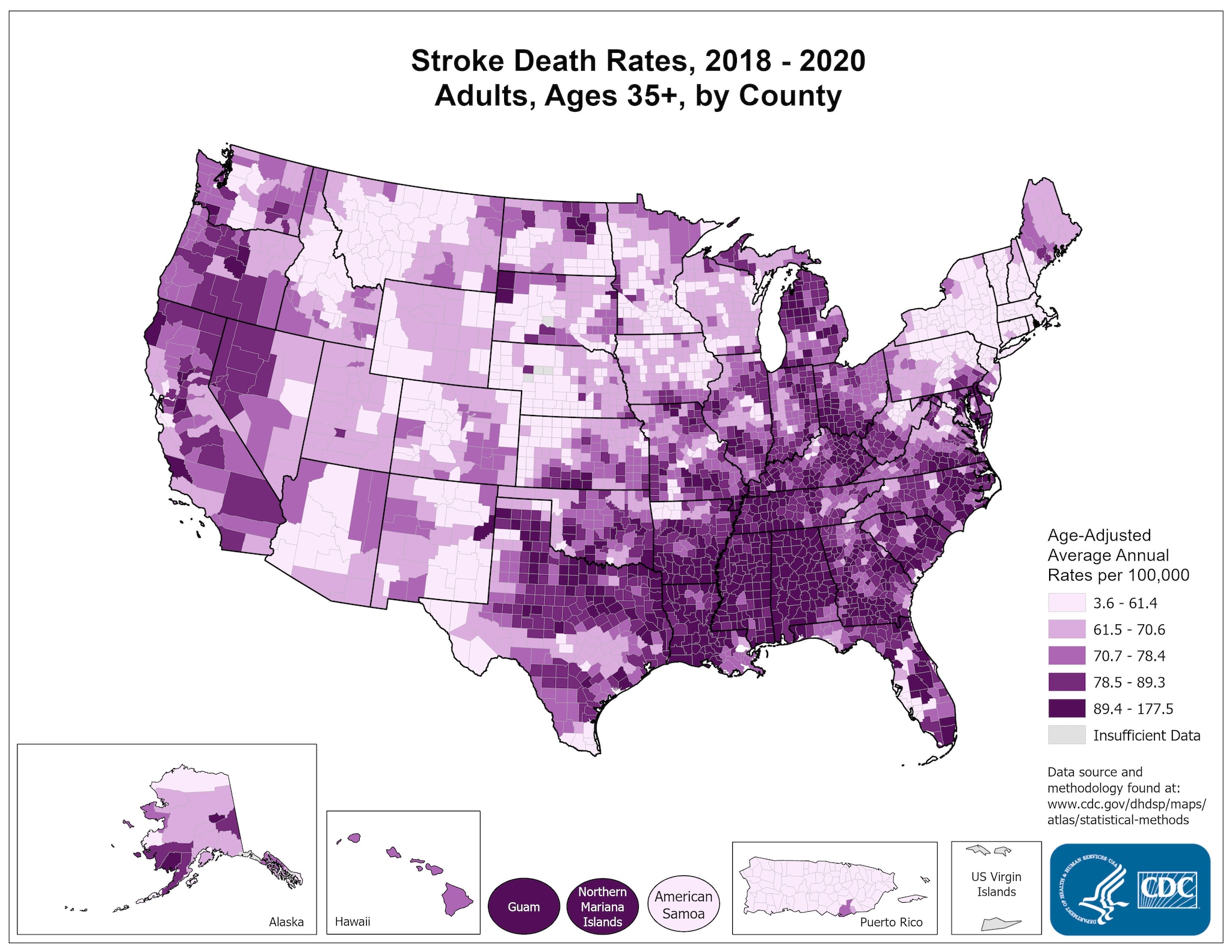
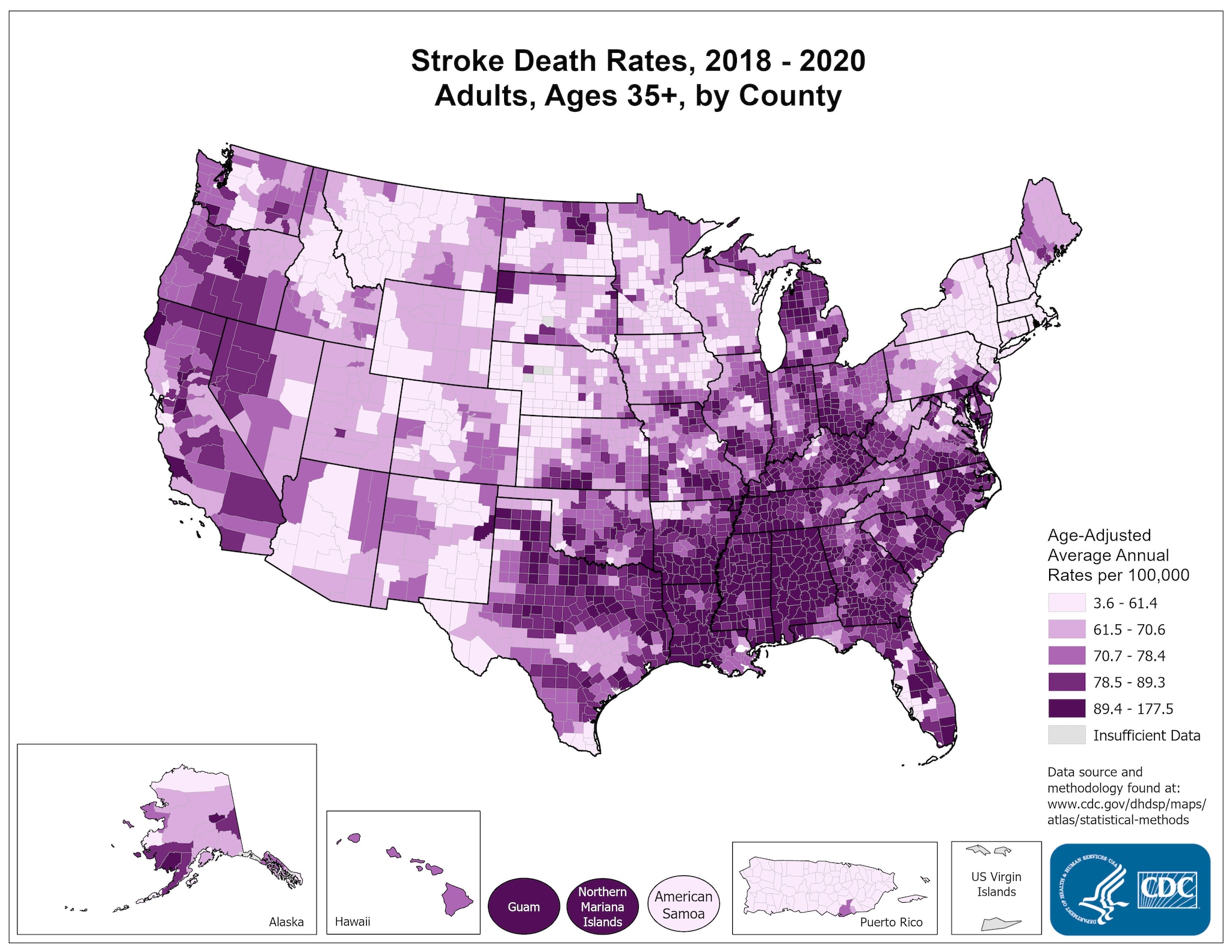
- Geography: Higher rates in the Southeastern U.S. (the so-called “Stroke Belt”), especially along the coasts in Georgia and the Carolinas (so-called “Stroke Buckle”).
- Heredity: Almost 2-fold higher among first-degree relatives. Chromosome 9p21 (proximal to genes CDKN2A and CDKN2B) has been linked to ischemic stroke risk
Prevalence - The Stroke Burden
For every 100,000 people in the UK there are 1,500 existing stroke cases and 1,000 with moderate disability following stroke. There is a wide variation worldwide and even within countries of stroke numbers. Stroke is probably under reported.
Racial
Black and Asian patients are more likely to have a greater risk of haemorrhagic strokes and to have them at a younger age group than whites. They have a greater incidence of hypertension and diabetes. Sickle cell is commoner in Black patients. White patients are more likely to have AF, smoke and take alcohol.
Socioeconomic
Those from lower income groups are more likely to have strokes and more severe strokes compared with those from higher income groups.
Stroke Belt
You may come across this US based term and it reflects a geographical spread of poor stroke mortality across a number of US states. It involves 11 US states and although there are many theories the exact cause has not been fully explained. The increased stroke risk is seen in both whites and blacks. There is a similar diabetes belt which covers the same area. Although many possible causes for the high stroke incidence have been investigated, the reasons for the phenomenon have not been fully determined.
Stroke mortality
Stroke does in itself produces a huge range of clinical severity from asymptomatic 'silent' disease found on imaging to patients who are moribund and die almost instantly due to massive brain infarction or haemorrhage. Not all strokes have a similar prognosis It is important when looking at stroke units or other clinical services that the variation in mortality between hospitals has perhaps more to do with the case mix in terms of stroke severity rather than the service provided. One needs to show that strokes of equal severity and equally matched patients are being compared. In the UK in 2000 there were 835 deaths per 100,000 (males) and of these 44 deaths per 100,000 attributable to stroke. Out of 559 deaths per 100,000 (females) there were 33 deaths per 100,000 attributable to stroke. The incidence of stroke has decreased in recent decades largely because of improved treatment of hypertension.
Stroke mortality varies mainly due to the severity of stroke (NIHSS and Oxford scales are useful) and comorbidities rather than care. Mortality also varies due to geographical areas, sex and races e.g. Stroke Mortality Rates in the USA. There is a wide variation worldwide and even within countries of stroke numbers. Stroke is probably underreported. Average death rate is 20-25%. In other parts of the world healthcare systems differ and modes of accessing care vary so this can affect the statistics.
| Stroke Mortality |
|---|
- 54/100,000 for white males
- 53/100,000 for white females
- 82/100,000 for black males
- 72/100,000 for black females
- 40/100,000 for Hispanics, American Indians and Alaskans
- 52/100,000 for Asian/Pacific islanders
|
Future Predictions
Despite the sobering statistics on stroke, there has been a steady reduction in stroke mortality since the 1950s across the world. The improvements are unlikely to be due to modern advances in stroke management but possible due to less severe strokes. All epidemiological data is only as robust in the methods for collection and diagnosis of stroke. Issues are whether studies cover both hospital and or community. Diagnostic methods - clinical or imaging and historical diagnoses. Certainly imaging and publicity over stroke is perhaps increasing pick up of those at the milder end of the spectrum.
Stroke mortality is also a difficult subject especially when restricted to inpatients. Mortality can vary depending on whether those with milder strokes which could be managed as outpatient are admitted and then counted. Mortality can be reduced by discharge to hospice or other care facilities so patients do not die as inpatients. Mortality can be reduced by excluding those who are dying, however this is less of a problem nowadays and stroke units should take all patients irrespective of immediate survival. There have been concerns that appropriate end of life care can increase 30 day mortality in patients in whom a more aggressive policy would have delayed the death beyond 30 days. This is controversial when some units are judged on their 30 day mortality as a quality indicator of care. The most important determinant in death from a stroke is by far the stroke itself and then severe co-existing illness.
The falling stroke mortality is excellent news but this is offset by the fact that an ageing population will mean that the absolute number of patients with stroke will rise in years to come. It is key then that we have coordinated strategies in place to help to reduce stroke risk, mortality and morbidity.
References and further reading