Learning objectives
- Learning
- Understand
- Integrate
- Reflect
|
The presence of brainstem atrophy in Neuro-Behcet's can be used as a powerful discriminator for the diagnosis
Introduction
- Behcet's disease is a multisystem, chronic-relapsing inflammatory disorder
- Its target is predominantly the venous system.
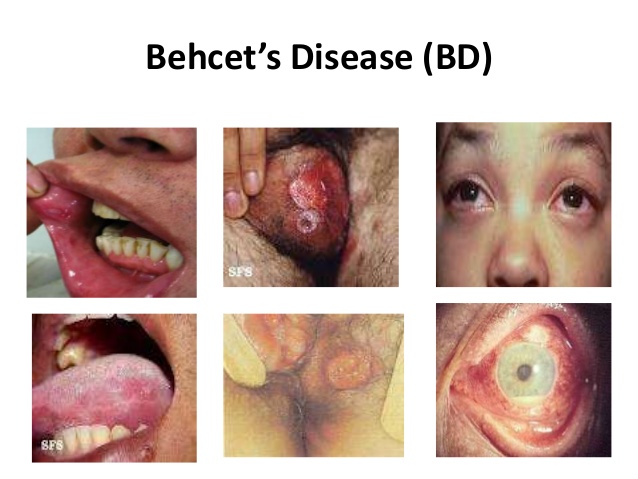
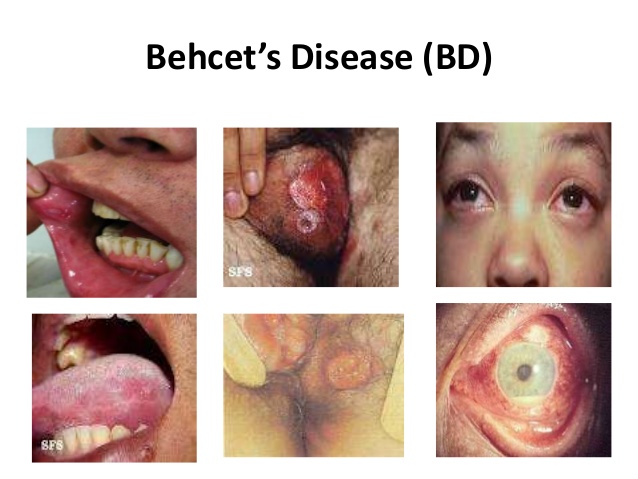
- triad of recurrent oral and genital ulcers with uveitis
Aetiology
- It is rare but commoner in the populations emanating from the Middle East, Far East and the Mediterranean.
- Brain involvement is seen in about a third with stroke and headache.
- There may be brainstem involvement. Cerebral venous sinus thrombosis may occur.
Clinical
- Painful recurrent oral and genital ulcerations
- Eye inflammatory changes such as uveitis and retinal vasculitis)
- Arthritis and painful muscles
- Venous thromboembolism may be seen.
- There are typical skin lesions (erythema nodosum) or a positive pathergy test result.
- However the diagnosis is entirely clinical as there is no definitive test.
CNS manifestations
- Focal or Multifocal CNS lesions: Seen in 5-20% of cases. Focal inflammatory lesions with corresponding neurology develops which can mimic stroke. This is the typical parenchymal type. The most common site is the brainstem. Diplopia, ataxia, dysphagia,pseudobulbar speech . Weakness and sensory symptoms. Spinal cord may be affected. Optic nerves can be affected.
- Meningoencephalitis: headache and drowsiness, which worsen over several days.
- Cerebral Venous thrombosis: Headache, ischaemic stroke with haemorrhage may be seen.
- Psychiatric: Rare cognitive and hallucinations and paranoia may develop. There may be fatigue, anxiety and depression
Differential
- Multiple sclerosis
- Neurosarcoidois
- Stroke disease
Investigations
- FBC, U&E, LFTs, CRP may be elevated
- The Pathergy test involves using a sterile needle to cause a small skin lesion which develops as a sign of skin hyperreactivity within 48 hours. False positive tests can be seen in pyoderma gangrenosum, Sweet syndrome, inflammatory bowel diseases, familial Mediterranean fever, acute myeloid leukaemia, and interferon alpha treatment.
- IL-6 cytokine : levels have been reported to correlate with disease activity in some
- MRI: changes typically may be seen in brainstem thalamic basal ganglia lesions. These can support the diagnosis of acute/subacute parenchymal disease. There may be focal or multifocal lesions. There may be signs of a meningoencephalitis. Lesions may show vasogenic oedema on T2. Cerebral vein thrombosis may be seen.
- CTV/MRV if suspected cerebral vein thrombosis
- CSF:shows more cells in parenchymal NBD and neutrophils might predominate
Criteria for diagnosis of Behcets
Mouth sores at least three times in 12 months and two of the following:
- Recurrent genital ulceration (including groin and anus, epididymitis, orchitis)
- Eye inflammation (iritis, uveitis, retinal vasculitis, cells in the vitreous)
- Skin lesions (papulopustules, pseudofolliculitis, erythema nodosum, acne in post-adolescents not on corticosteroids) ?
- Pathergy (raised erythematous papule at site of needle prick 24 to 48 hours or more later)
Management
- Local steroid preparations may be used for ulcers and Colchicine is used for orogenital disease
- Eye involvement needs urgent ophthalmologist review and is treated with steroid eye drops, injections, azathioprine, or biologic drugs such as infliximab or interferon.
- Referral to a neurologist experienced in management of the CNS manifestations of the disease is recommended.
- Anticoagulation for those with Cerebral Venous thrombosis
- In those with CNS involvement high dose IV Methylprednisolone and immunosuppressives may be used. Long term azathioprine, methotrexate or mycophenolate.
- In aggressive disease cyclophosphamide and methotrexate and interferon-alpha, or azathioprine may be considered.
- Biological agents may also be considered such as infliximab or etanercept.
References