Learning objectives
- Learning
- Understand
- Integrate
- Reflect
|
Pathophysiology
- An ischaemic stroke may be due to an obstructed artery or arteriole or occasionally a vein
- Arterial occlusion are divided into large vessel (LCA/PCA/ACA) and small penetrating artery (lacunar) strokes
- Occasionally there is no obstruction but a stroke has been caused by low flow which may be transient or fixed.
- If the reduction in flow was long enough infarction can result.
- May be seen due perhaps to systemic hypoperfusion usually affecting the so called watershed areas between arterial zones and often in those with pre-existing stenoses e.g bilateral carotid artery stenosis.
- Once blood flow dips below a critical level for more than a few minutes then infarction occurs.
- Usual supply is 50 ml/100 mg/min of brain tissue when brain is "at rest".
- Below this changes are seen which are initially reversible but at a certain point become irreversible and cell death is noted.
- It's a good time to just also remember the concept of penumbra.
- When blood flow is reduced a core around the perfused artery which is obstructed will infarct but a surrounding area will just experience reversible changes if flow is re-established.
- This is the penumbra and is the volume of the brain that we attempt to salvage with modern reperfusion strategies.
Radiological appearance of Infarction
 |
 | 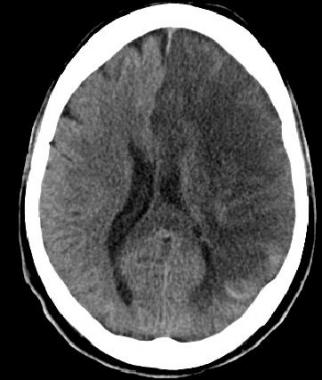 |  |
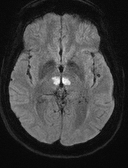
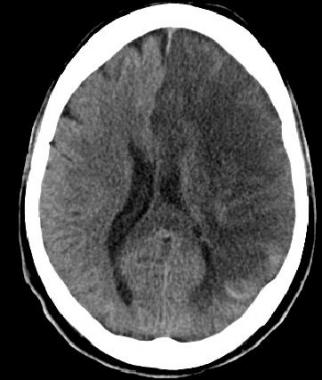
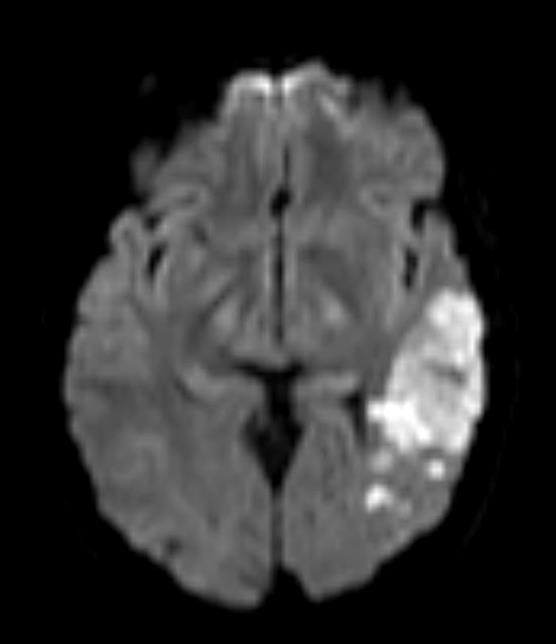
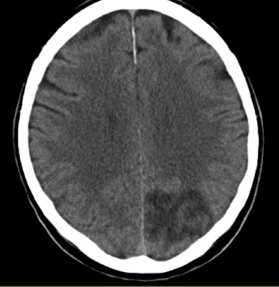
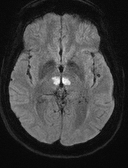
| Bilateral Thalamic Infarction(AOP) | Dense Left MCA | Subacute Left ACA/MCA infarct | Old Right Parietal Infarct (MCA) |
|---|
 | 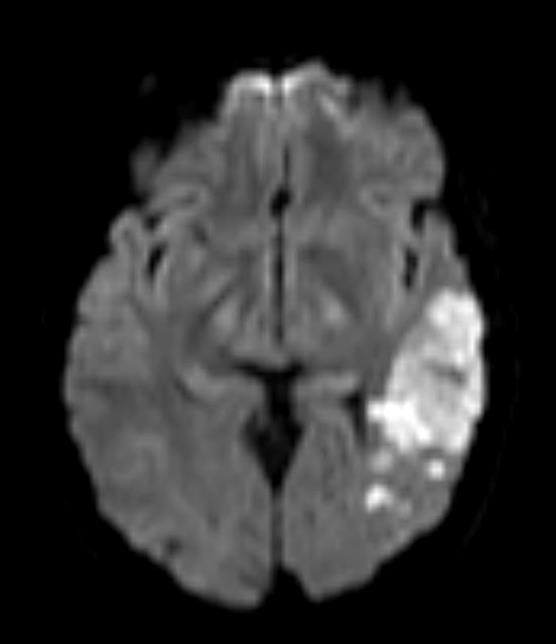 | 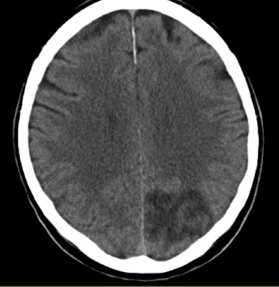 |
| Lacunar strokes (Small vessel) | Branch of the Left MCA | Left PCA infarct |
|---|
| Mechanisms of Infarction |
|---|
- Large artery atherosclerotic plaque rupture or a dissection and occlusion e.g. internal carotid artery
- Large artery embolic obstruction due to clot from heart or artery to artery thrombus migration or paradoxical embolism
- small-vessel occlusion due to lipohyalinolysis
- Watershed due to reduced flow that leaves the edges of arterial territories underperfused
- Venous infarction - obstructed venous drainage leads to ischaemia and sometimes haemorrhage
- Cryptogenic - there are some diseases and the mechanism of infarction is very poorly understood and no cause can be found.g. migrainous infarction
- Metabolic defect resulting in cell dysfunction and death e.g. MELAS
|
A word of caution is that things are not always as clear cut as it seems. I have certainly had patients with quite evident large vessel disease e.g. severe ipsilateral carotid disease who seem to have sustained a lacunar type infarct which one presumes was small vessel. Has a thrombus or plaque blocked the ostia of a perforating branch. Difficult to explain. There are theories why this may happen but it is a good point to say that one cannot always be completely confident as to aetiology. There are always the exceptions that can trip us up.
Pathophysiology of Ischaemic Stroke
- Can also be thought of at more fundamental what actually happens and where and why. This is an attempt at a more anatomical level of aetiology. It is certainly not exhaustive. In summary the causes can be seen as arterial and venous thrombosis, embolism and low flow. Your understanding of stroke will improve if you refresh the anatomy of the pathway of blood from the heart to the brain. The anterior circulation is the brain supplied by branches of the carotid artery. In health the external carotid provides no significant supply to the brain. The posterior circulation is the brain supplied by branches of the vertebral artery.
- Carotid Arteries: Both ascend and bifurcate at the level of the thyroid into internal and external carotids. The internal carotids ascend through the base of the skull and through the cavernous sinus and then emerge to split into anterior and middle cerebral arteries.
- Vertebral Arteries: The vertebral arteries are the first branch of the subclavians arteries. They ascend and pass into the foramina on the cervical cord and enter the skull through the foramen magnum in front of the spinal cord. They ascend and fuse to form the basilar artery at the pontomedullary junction. The basilar lies in front of the pons and then splits again into the right and left posterior cerebral arteries at the midbrain level. Theses sweep back around the brainstem to pass to the occipital cortex.
Aetiology of Ischaemic Stroke
1.Thrombotic Strokes
First review a few basics. Fibrin is a protein whose tertiary and quaternary qualities lend it to form a mesh that can form a physical structure that can stop bleeding. It is derived from fibrinogen. The serine protease enzyme thrombin converts fibrinogen to fibrin. A clot is formed. Eventually the body breaks down the clot - 'fibrinolysis' and the clot is removed. On the surface it seems simple but the reality is a complex interconnected set of events. First lets deal with some of the important players in thrombosis. Note that thrombosis can include venous infarction as well as arterial.
2. Embolic strokes
Sources of Emboli to Internal Carotid/Vertebral or Circle of Willis Branch
- Pre-Cardiac Origin : DVT/Pelvic vein thrombus via ASD/PFO/Atrial septal aneurysm to Left atrium - Paradoxical embolisation
- Left Atrium: LA or LA appendage thrombus with AF or LA myxoma (raised ESR)
- Mitral valve: Infective endocarditis, Libman sacks endocarditis, Myxomatous valve, Prosthetic valves : Metal >> Tissue
- Left Ventricle: LV thrombus, Myocardial infarction and mural thrombus, Cardiomyopathy
- Aortic Valve: Infective endocarditis, Degenerative/Calcifications, Prosthetic valves: Metal >> Tissue
- Aortic arch: Atheromatous plaques, Calcifications, Aortic dissection, and overlying thrombus
- Common Carotid and Internal Carotid artery to Internal Carotid, ACA and MCA: Atheromatous plaques, Calcification, Dissection and overlying thrombus
- Vertebral to Vertebral, Basilar arteries and PCA branches: Atheromatous plaques, Calcification, Dissection and overlying thrombus
3. Low flow strokes
- Transient hypotension causing watershed strokes between vascular territories
- ACA and MCA interface
- MCA and PCA interface
- Often symmetrical/bilateral
- Bilateral carotid artery stenosis and hypotension
- Subclavian steal syndrome
Ischaemic Strokes Distribution
This data comes from the Lausanne Stroke Registry of 1000 patients screened with CT which were repeated if initially normal. This may now be different with the increased use of MRI
| Anterior Circulation(Carotid territory) 68% |
|---|
- MCA 98% (Entire 13%, Deep 32%, Anterior superficial 31%, Posterior superficial 20%)
- ACA 3%
- Internal carotid 1%
|
| Posterior Circulation (Vertebrobasilar territory) 26% |
|---|
- Brainstem 48% : Pons 27%, Medulla 14%, Midbrain 7%
- Cerebellum 7%
- PCA territory: Entire 7%, Deep 11%, Superficial 18%, Multiple 9%
|
| Others 26% |
|---|
- Watershed (low flow) infarction 3%
- Multiple sites 3%
|