Learning objectives
- Learning
- Understand
- Integrate
- Reflect
|
Introduction
It is not uncommon for us to diagnose brain tumours either in the TIA clinic or the Emergency department. The usual presentation is usually of progressive symptoms and development of weakness which is not completely de novo. If there is a history and imaging corresponding to that suggesting a tumour thrombolysis must be avoided. Occasionally tumours present with haemorrhage and then it can be difficult to differentiate from a haemorrhagic stroke but in most cases acute or delayed imaging will help with the diagnosis. Meningiomas are tumours that arise outside the brain "extra-axial" but can cause localised pressure with oedema affects the underlying. There are two main types of tumour. Those that arise from the brain itself called primary tumours. The most common are usually from glial cells and known as gliomas. Secondary tumours are those that spread to the brain from elsewhere. For a single lesion it can be primary or secondary. If there are multiple lesions they are usually from elsewhere.
Different types
- Secondary: Commonest. Often Breast, Lung, Colorectal, Thyroid, Testicular, Renal cell and malignant melanoma
- Primary brain: Glial cells - Gliomas : Milder Astrocytomas to aggressive Glioblastoma multiforme, Meningioma, Oligodendroglioma
- HIV related : non-Hodgkin's lymphomas of B-cell type
Imaging
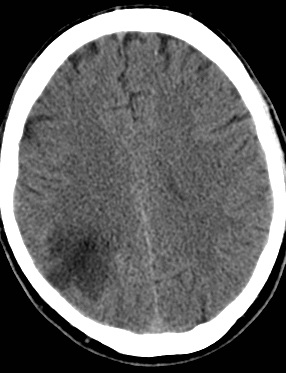
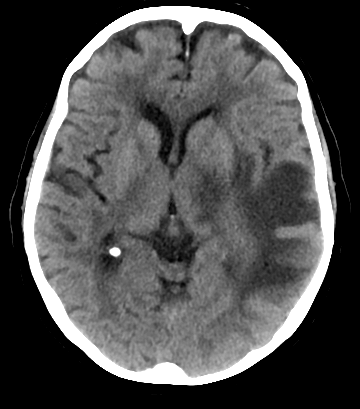
Solitary tumour

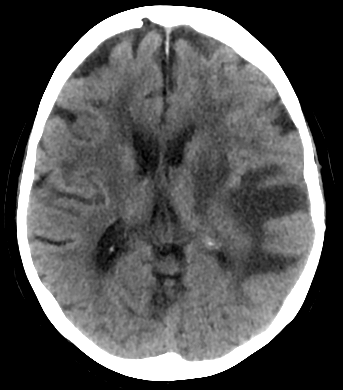
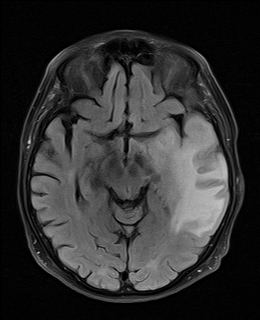
Haemorrhagic Metastases

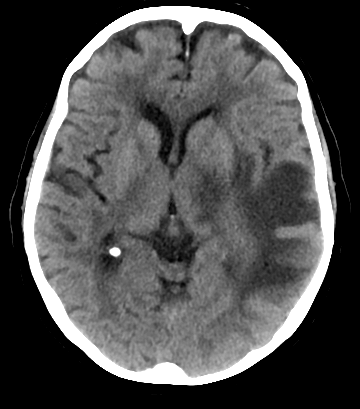
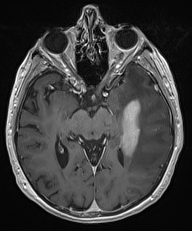
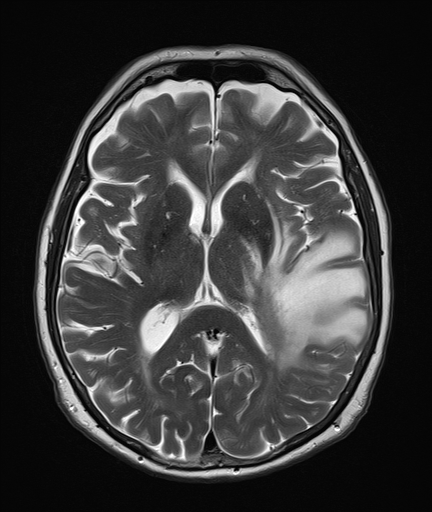
Cerebellar metastases
Primary Tumours
- Primary brain tumours can be defined as benign or malignant growths arising from intracranial tissue.
- There is a wide spectrum of severity with operable benign tumours to inoperable malignant lesions
- Relatively uncommon and forms 2% of adult tumours.
- Can affect all ages and both sexes, increasing in incidence with age
- Women have a higher incidence of meningioma than males.
- Tumours need to be classified pathologically, and staged to determine treatment and prognosis.
- Approximately half are benign.
- Most common malignant primary brain tumour is glioblastoma multiforme (GBM) which has a poor prognosis.
Gliomas
| Astrocytomas are the most common type of glioma and are graded according to the
WHO scale of grades one to four. |
|---|
- Grade 1: astrocytomas include pilocytic astrocytomas which are benign.
- Grade 2: astrocytomas are low grade infiltrating tumours.
- Grade 3: anaplastic astrocytomas exhibit mitoses.
- Grade 4: glioblastoma multiforme(GBM) is the most aggressive primary brain tumour
|
GBM has a median survival of 14 months following diagnosis even if given optimal therapy. GBM can arise as a first presentation or a secondary presentation to a lower grade astrocytoma.
The gliomas most commonly encountered in adults are neoplasms of astrocytic or oligodenrocytic lineage. Mixed tumours also occur, the most common of which is
termed anaplastic oligoastrocytoma. Glioblastomas form around 50% of these tumours. Others include oligodendrogliomas, other
astrocytomas and ependymomas.
Meningiomas
Meningiomas arise from the meninges and often compress the brain thereby creating a mass effect. Incidence is 2 per 100,000. They are benign and are
therefore potentially curable through resection. Loss of chromosome 22 is a characteristic genetic feature of these tumours. They are vascular and enhance with gadolinium.
Primary CNS lymphoma
Primary CNS lymphoma is another tumour within the grouping of non-gliomas. They form 2-3% of total brain tumours in people of normal immunity. Patients with
immunodeficiency e.g. HIV are at an increased risk of developing this form of cancer
Clinical
- Symptoms due to local effects and general rise in ICP
- Childhood tumours are mainly posterior fossa which present with hydrocephalus
- Headache - worse in morning and on stopping/straining
- Changed personality, Seizures
- Stroke like episodes when tumour bleeds or causes focal seizure activity
- Coma due to Raised ICP/Hydrocephalus or Seizure or haemorrhage
Investigations
- FBC, U&E, LFTs, ESR, CRP. HIV test may be indicated.
- CXR: exclude lung cancer
- Tumour markers may be useful : Alpha fetoprotein (testicular cancer), CEA (colorectal, pancreatic, breast), CA125 (breast), S-100 (melanoma), PSA (prostate)
- CT with contrast: There is breakdown of the blood brain barrier such that tumours enhance with contrast. This often shows up with a surrounding area of oedema.
- MRI with gadolinium: There is breakdown of the blood brain barrier such that tumours enhance with gadolinium. This often shows up with a surrounding area of oedema.
- Look for primary : Usually a CT Chest Abdomen and pelvis. Physical exam and Mammography for breast cancer and skin examination for melanoma.
- Brain biopsy: When a tumour is identified by imaging it can then be biopsied to obtain a definite tissue diagnosis, so as to
better inform the MDT as to how best to proceed with treatment.
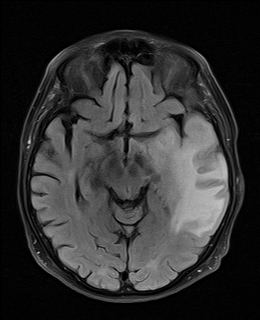
Difficulties of Diagnosis Tumour vs Stroke
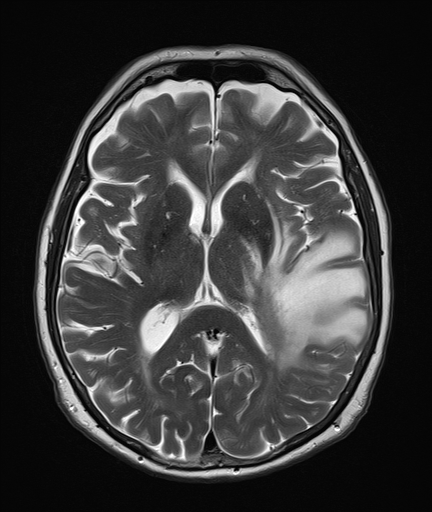
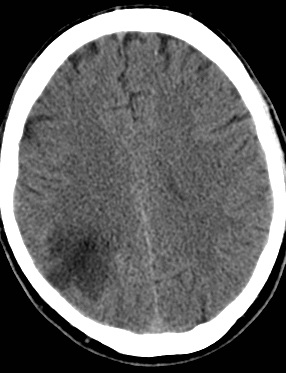
 | Day 1: admitted suspected stroke but some atypical features.
Patient improved and discharged home |
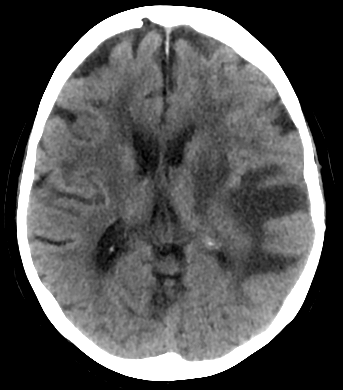 | Day 15: clinical worsening |
 | Day 18: clinical worsening |
 | Day 21 |
 | Day 21 |
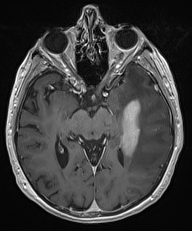 | Day 21 |
 | Day 21 with contrast |
Management
Surgery is often but not always considered which can help
- Surgeons to obtain a histological diagnosis
- Reduce the mass of the tumour reducing the neurological deficit
- To treat hydrocephalus if present
- Surgery can be curative for benign tumours
- Surgery may simply debulk tumour and leave behind residual tumour and this may be palliative
Surgery involving the brain is always high risk and any situation can be made worse through surgical and perioperative complications. A full discussion with the neurosurgeon and anaesthetists is needed before any intervention is planned with a good discussion of risks and benefits.
Specific Management
- Neurosurgical Debulking can improve the prognosis for malignant tumours provided the tumour is not infiltrating essential "eloquent" areas of the brain such as language areas. If this is not possible then simple biopsy is the second option and modern stereotactic approaches mean that this is now more possible. Excision of at least 98% of a GBM improves life expectancy by a median of 4 months compared with patients who have 2% or more of residual tumour remaining post operatively.
- Chemotherapy is increasingly being used in the treatment of primary brain malignancies. Temozolamide, an alkylating agent which has good penetration of the blood brain barrier thereby allowing access to brain tissue. Certain regimens in combination with radiotherapy have shown a survival benefit in gliomas compared to controls. Chemotherapy can be used also in the treatment of oligodendrogliomas
- External beam radiotherapy is useful and may be used in addition to surgery or instead of surgery. Some tumours are radiosensitive and it can be curative or prolong survival. Whole
brain radiotherapy is used in certain tumours like medulloblastoma and primary CNS lymphomas. “Involved field” radiotherapy is used in other tumours such as gliomas.
- Stereotactic radiosurgery is another method of radiotherapy, which delivers a large dose of radiation to the tumour based on imaging of the lesion. This is useful for meningiomas.
- Referral to local neuro-oncology services. Oncology can discuss with Neurosurgeons whether to biopsy, remove or resect lesion.
- Much of this focuses on performance status, co-morbidities and physiological age and whether an eloquent area of the brain is involved and the scope for resection and patient choice.
- Start anticonvulsants e.g. Keppra 250-500 mg BD with one seizure as high risk of recurrence with a focal lesion.
- Hydrocephalus is an emergency that requires transfer to the Neurosurgeons for shunting
- Start Dexamethasone 10 mg IV and Dexamethasone 4 mg PO/IV QDS which can be increased to reduce oedema
- For many palliation is the correct course when there is a poor outcome.
- It is generally agreed that a high rate of recurrence in brain tumour is due to the resistance of a sub-population of cancer stem cells