Learning objectives
- Learning
- Understand
- Integrate
- Reflect
|
Introduction
- Malignant MCA syndrome may be seen following a large MCA territory infarct.
- It usually occurs 2-5 days post onset of stroke but sometime can occur earlier within 24 hrs.
- There is localised cytotoxic oedema, swelling and often midline shift.
- Trials have shown that surgery both reduces mortality and improves functional status but also results in the survival of more patients with severe disability.
Aetiology
- MCA occlusion may be due to atheroembolism
- Cardio embolism from AF or structural cardiac disease
- Carotid dissection may embolise to the MCA
Clinical
- Left/Right MCA syndrome
- Progressive reduced level of consciousness
- Pupillary changes and Cheyne-Stokes respiration
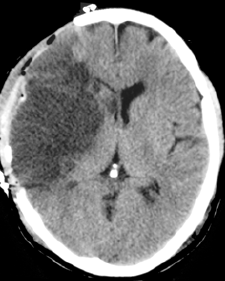
Images
Investigations
- CT scan initially may be normal or show a hyperdense artery. Overtime there is progressive hypodensity and obvious cytotoxic oedema and midline shift.
- MRI will show infarct volume and extent
| RCP Guidance 2016 |
|---|
Patients with middle cerebral artery (MCA) infarction who meet the criteria below should be considered for decompressive hemicraniectomy. Patients should be referred to neurosurgery within 24 hours of stroke onset and treated within 48 hours of stroke onset:
- Pre-stroke modified Rankin Scale score of less than 2
- Clinical deficits indicating infarction in the territory of the MCA
- National Institutes of Health Stroke Scale (NIHSS) score of more than 15
- A decrease in the level of consciousness to a score of 1 or more on item 1a of the NIHSS
- signs on CT of an infarct of at least 50% of the MCA territory with or without additional infarction in the territory of the anterior or posterior cerebral artery on the same side, infarct volume greater than 145 cubic centimetres on diffusion-weighted MRI
|
Management
- Even with ICP management with endotracheal intubation, blood pressure control, osmotherapy, hyperventilation, and barbiturate anaesthesia for refractory intracranial hypertension, mortality rates of up to 80% have been reported.
- Decompressive hemicraniectomy with durotomy involves the removal of a large flap of bone and the layer of dura that lies over the brain. The brain can herniate beyond the confines of the skull. The result is that brainstem compression is less likely, and survival increased.
- Patient selection will depend upon the patient's known views and wishes as to how they would wish to be managed. A poor functional baseline with significant co morbidities may suggest surgery is not in the patient's best interests. Involvement of the PCA and/or ACA on imaging would suggest a poorer outcome. AN infarct volume > 145 cm on DWI is also associated with poorer outcomes.
- There was previously a cut off age of 60 but the DESTINY II trial of decompressive hemicraniectomy for older patients showed a substantial survival benefit for patients over the age of 60 years (Juttler et al, 2014) akin to that seen in young patients (Cruz-Flores et al, 2012). Decisions to undertake major life-saving surgery need to be carefully considered on an individual basis, but patients should not be excluded from treatment by age alone
References