Learning objectives
- Learning
- Understand
- Integrate
- Reflect
|
Opalski felt that weakness was due to ischaemia of the lateral medulla to the upper cervical cord involving corticospinal fibres caudal to pyramidal decussation. May also be occlusion of the posterior
spinal artery
Introduction
- All arterial strokes produce vascular syndromes and Lateral Medullary syndrome is no exception.
- Named after Adolf Wallenberg a German in 1895 but was first described in 1808 by Gaspard Vieusseux
- Opalski syndrome (1946) is considered a variant of Wallenberg syndrome with ipsilateral hemiparesis
- Aetiologies can be mixed and varied small and large vessel
Aetiology
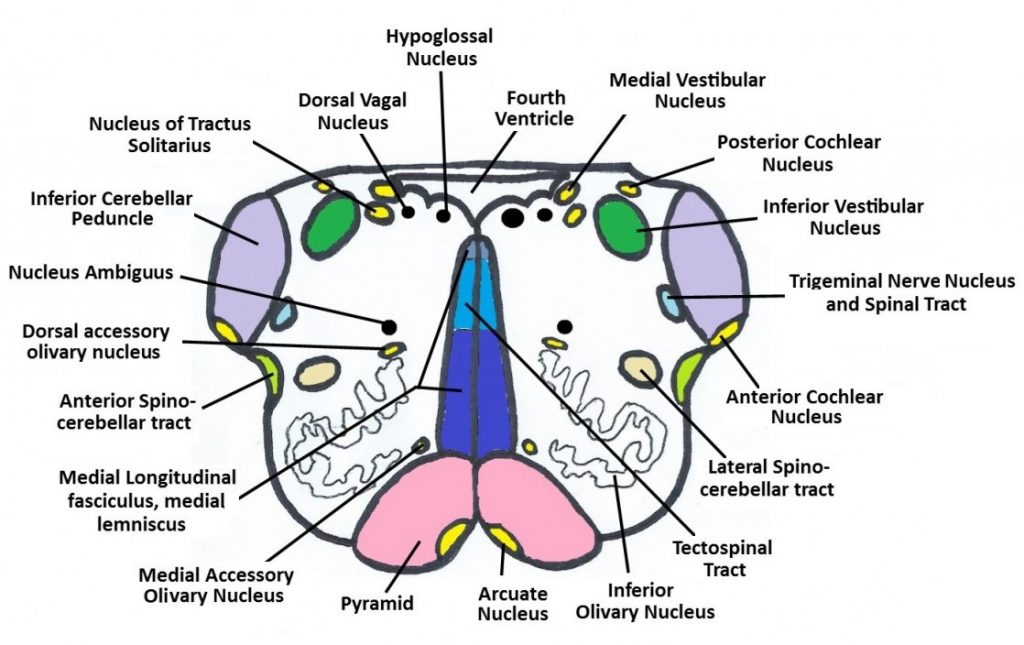
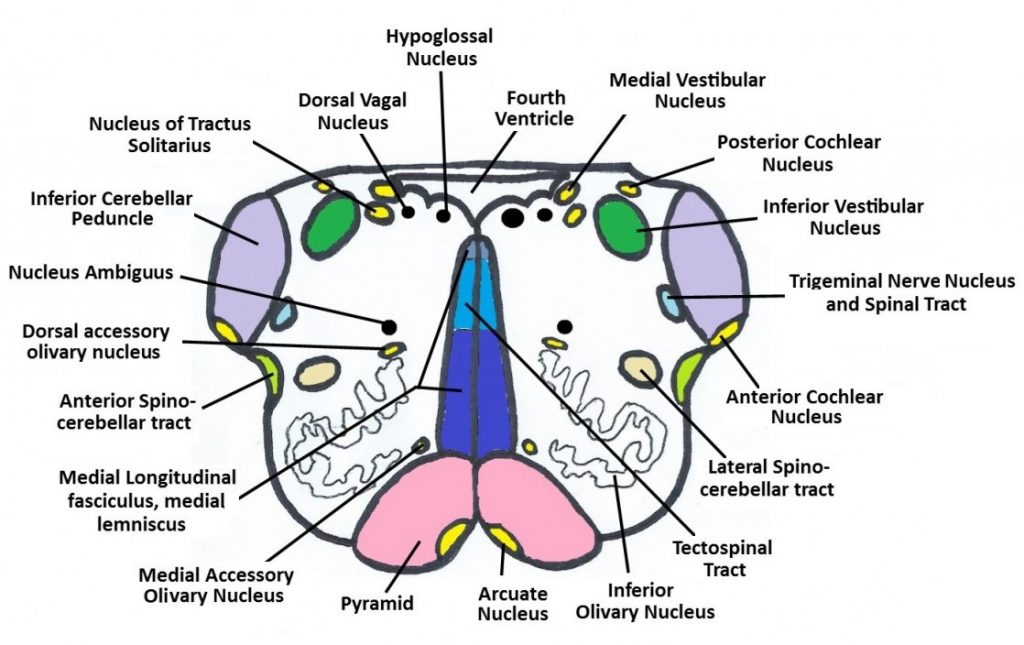
- Medulla packed with important long fibre tracts
- Occlusion of vertebral artery (VA)
- Occlusion of Posterior inferior cerebellar artery (PICA)
- Occlusion of small lateral medullary perforators
- Cardio embolism, Atherosclerosis, Dissection, Moyamoya disease etc.
Clinical
- Sudden loss of swallow (Nucleus Ambiguus)
- Ipsilateral Ataxia/Dysmetria/Truncal/Dysarthria instability: Lateral cerebellum or inferior cerebellar peduncle
- Horner's syndrome: Small pupil and mild ptosis on same side as lesion
- Ipsilateral hemiparesis (Opalski syndrome)
- Ipsilateral reduced facial sensation to pain and temperature: Descending nucleus of V
- Contralateral reduced arm/trunk/leg sensation to pain and temperature : Spinothalamic tract
- Hiccups: May be a vagal mediate phenomenon
- Vertigo: vestibular nucleus
- Respiratory distress and apnoea
- Aetiological clues: Neck pain/trauma with dissection, AF, HTN, smoking, alcohol

Investigations
- FBC, U&E, LFTs, ESR, ECG, CXR
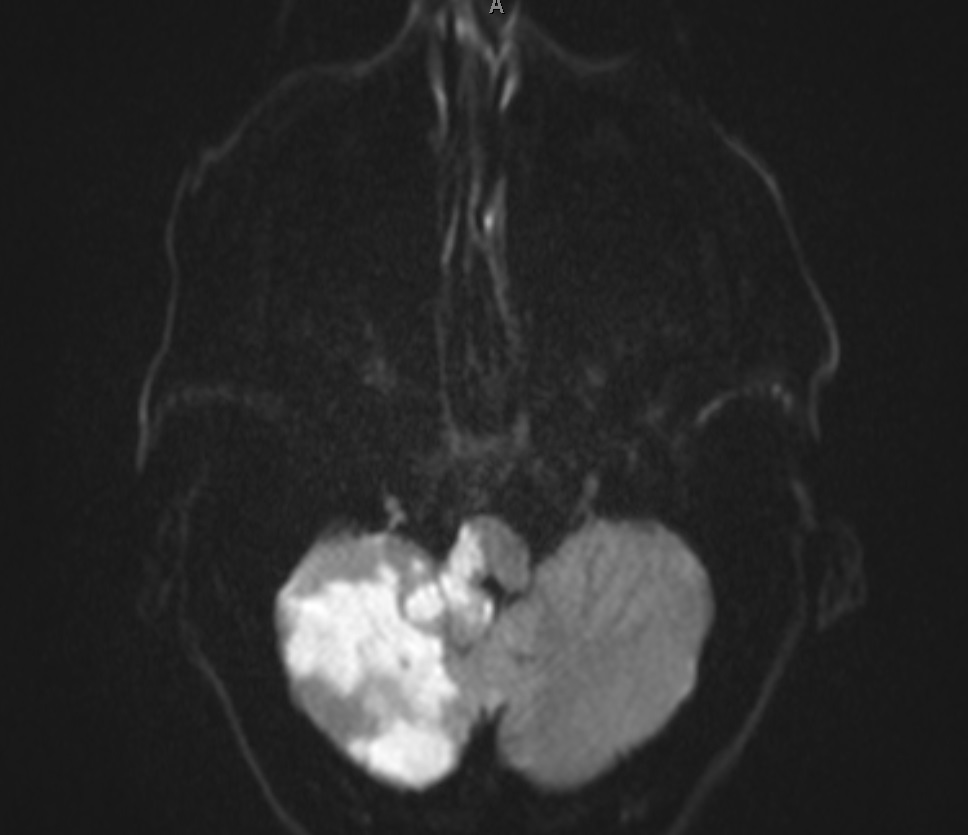
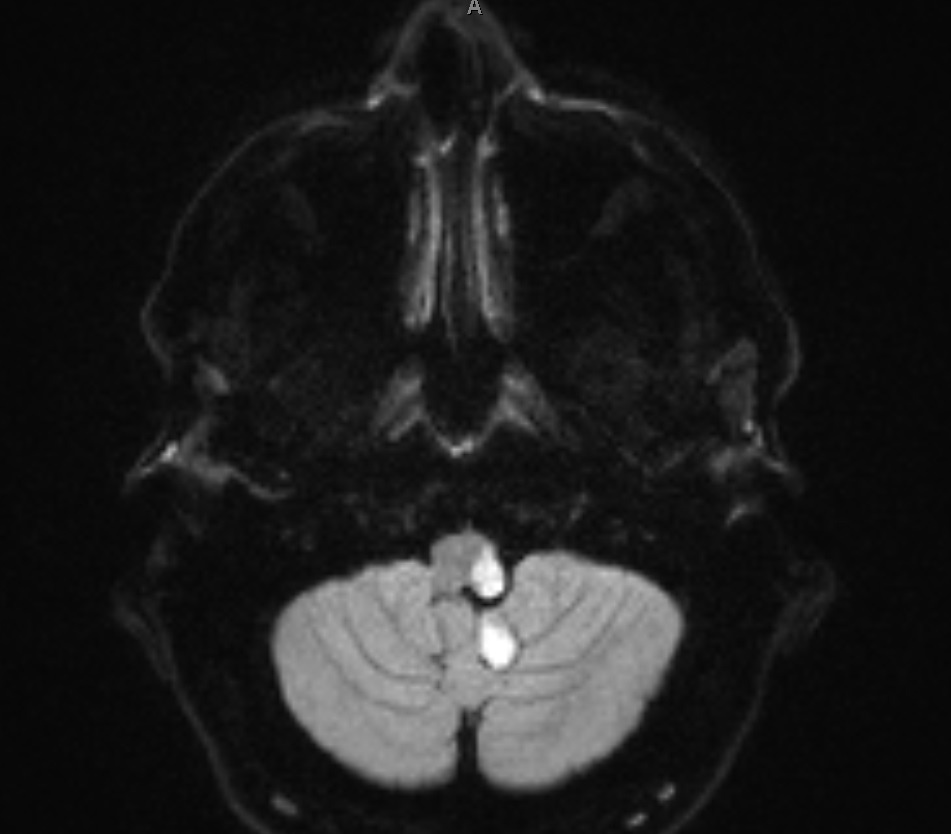
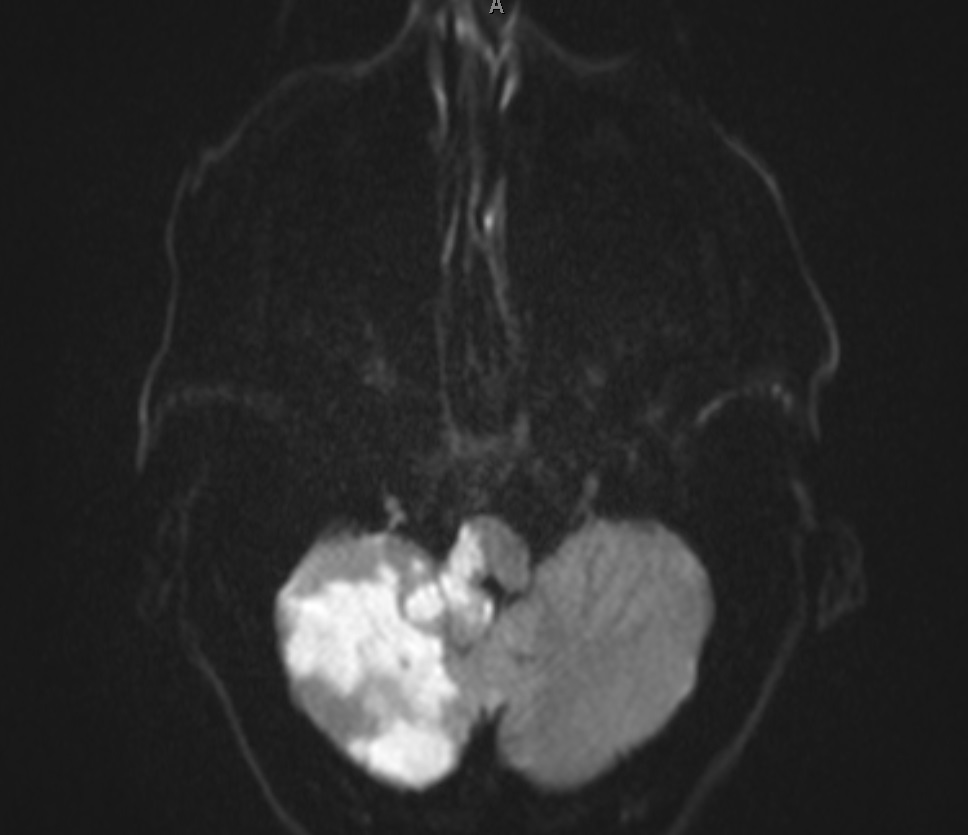
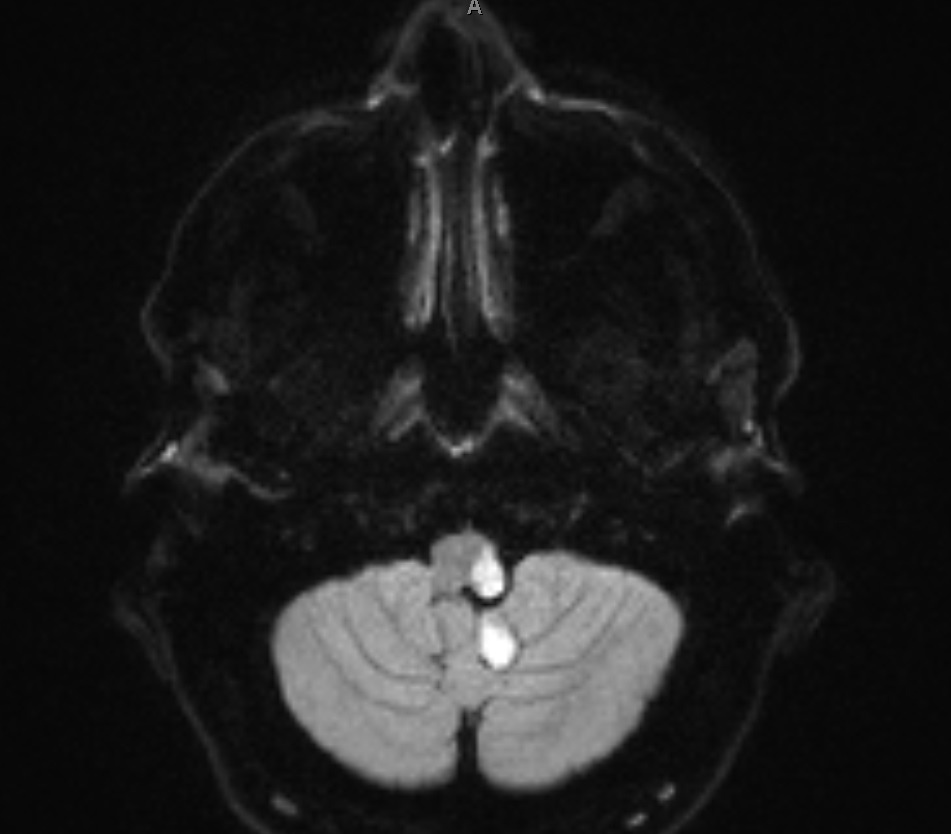
- MRI is diagnostic and the lesion should be visible but can be missed if not actively looked for or the MR has not gone low enough
- MRA/CTA may be done to assess vasculature or if dissection suspected
- Echocardiogram and 24 hr or 7 day tape
Management
- ABC. Some may rarely have respiratory distress and apnoea and may need intubation and ventilation.
- Assessment for thrombolysis. Often the NIHSS under reports the disability. I have certainly thrombolysed people with the syndrome with loss of swallow (but a borderline NIHSS) which is often one of the most disabling features.
- Aspirin 300 mg for 14 days with a PPI if needed.
- If swallow impairment goes on for over 2 weeks then a PEG may allow earlier discharge
- Ongoing Hiccups - Try Chlorpromazine 25-50 mg 6 hrly or Metoclopramide 10 mg PO TDS
- Long term Clopidogrel and Statin and as this can be a large vessel stroke due to VA occlusion then looking for AF and other sources of emboli is reasonable.
References