Learning objectives
- Learning
- Understand
- Integrate
- Reflect
|
FMD will do one of four things to arteries - stenosis, aneurysm, dissection, or occlusion
Introduction
- Fibromuscular dysplasia (FMD) is an idiopathic disease of small- and medium-calibre arteries.
- The disease can affect all the layers of the artery causing an angiopathy.
- It tends to affect the distal extracranial portion of the carotid artery.
- Commoner in young and middle aged females. Female > male incidence is about 3:1.
- It can be a cause of stroke in childhood
Aetiology
- Has been found in 1% of carotid arteries at post mortem.
- It is segmentary, non-inflammatory and non-atherosclerotic
- Causes both stenosis and/or dilation of blood vessels.
- Consider diagnosis in young patients with ischaemic stroke or with saccular aneurysms +/- SAH.
Classification
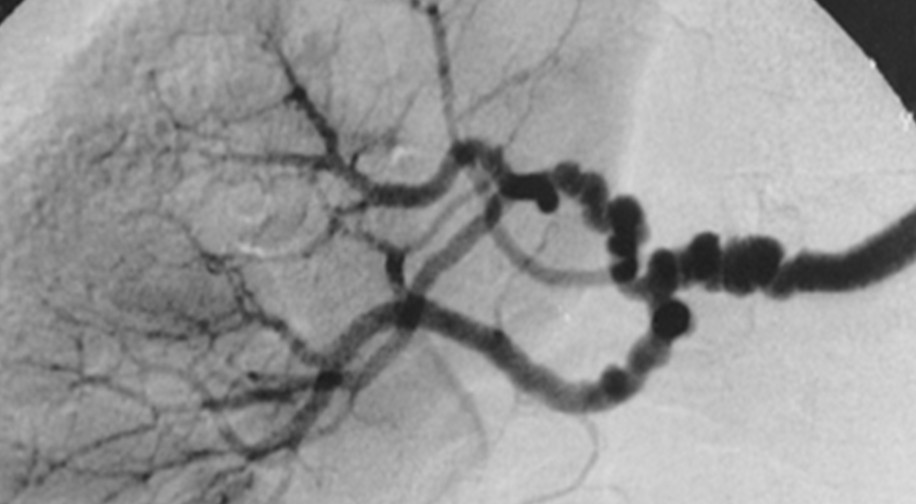
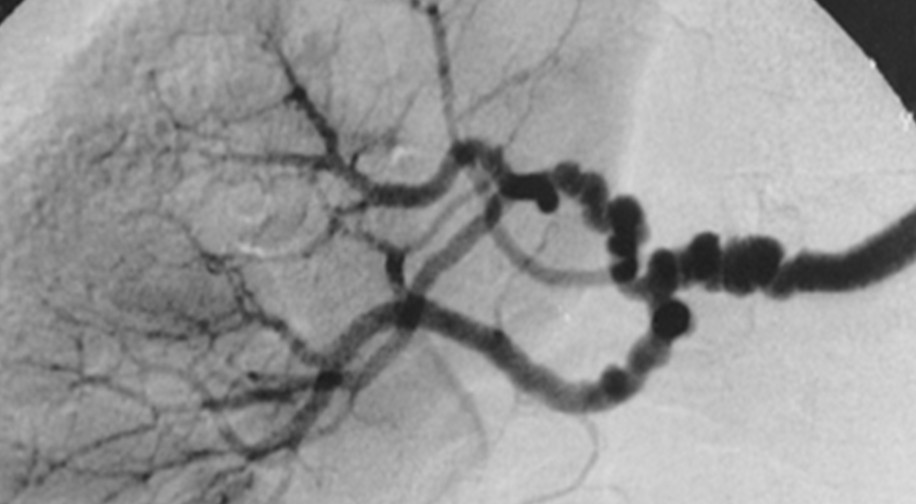
- Medial fibroplasia (80%): Commonest form. Classical beading appeanace on angiogrpahy. The multiple stenotic “webs” cause arterial stenosis and poststenotic dilation. Aneurysms are often seen.
- Intimal fibroplasia (10%): Collagen deposition within the intima with damage to internal elastic lamina. Angiography a fibrotic band-like constriction or long tubular lesions
- Perimedial fibroplasia(<10%): Young girls aged 5-15 with hypertension and renal impairment
- Medial hyperplasia (<1%): Pathologic diagnosis.
- Adventitial fibroplasia (< 5%)Can be diagnosed using intravascular ultrasound (IVUS) imaging. Angiography resembles intimal disease.
Clinical
- Carotid or vertebrobasilar infarction
- Carotid Dissection
- Vertebral Dissection
- Renal Artery Stenosis causing refractory hypertension
- Carotid Stenosis +/- stroke
- Spontaneous Coronary artery dissection (SCAD)
- Can affect pulmonary arteries
- Subarachnoid haemorrhage
Investigations
- FBC, U&E, Creatinine: look for renal impairment
- CT/MRI may show infarction or SAH
- CTA/MRA/DSA : Narrowing and bead-like dilatations of artery seen on Angiography. Arterial dissection. Coexistence of saccular aneurysms
- Post mortem: vascular histology shows increased collagen within the intima and media. The media may be thinned and there may be beading.
- No specific genetic or antemortem tests
Management
- As per normal Ischaemic stroke.
- Manage dissection usually with antiplatelets short/long term.
- Intervention for Renal artery stenosis may be useful.
- Antihypertensive medications if hypertensive
References and recommended reading