Learning objectives
- Learning
- Understand
- Integrate
- Reflect
|
Introduction
- This is a lower motor neurone weakness of facial nerve typically unilateral and is named after Sir Charles Bell (1774-1842).
- Incidence of Bell's palsy is 15 to 30 per 100,000 persons. Equal numbers of men and women affected.
- It is important for stroke physicians to diagnose this or it can lead to over investigations and overdiagnosis as potential stroke.
Aetiology
- Most are idiopathic though many suspect a viral aetiology though aciclovir has not been shown to change outcome so possibly not HSV/VZV.
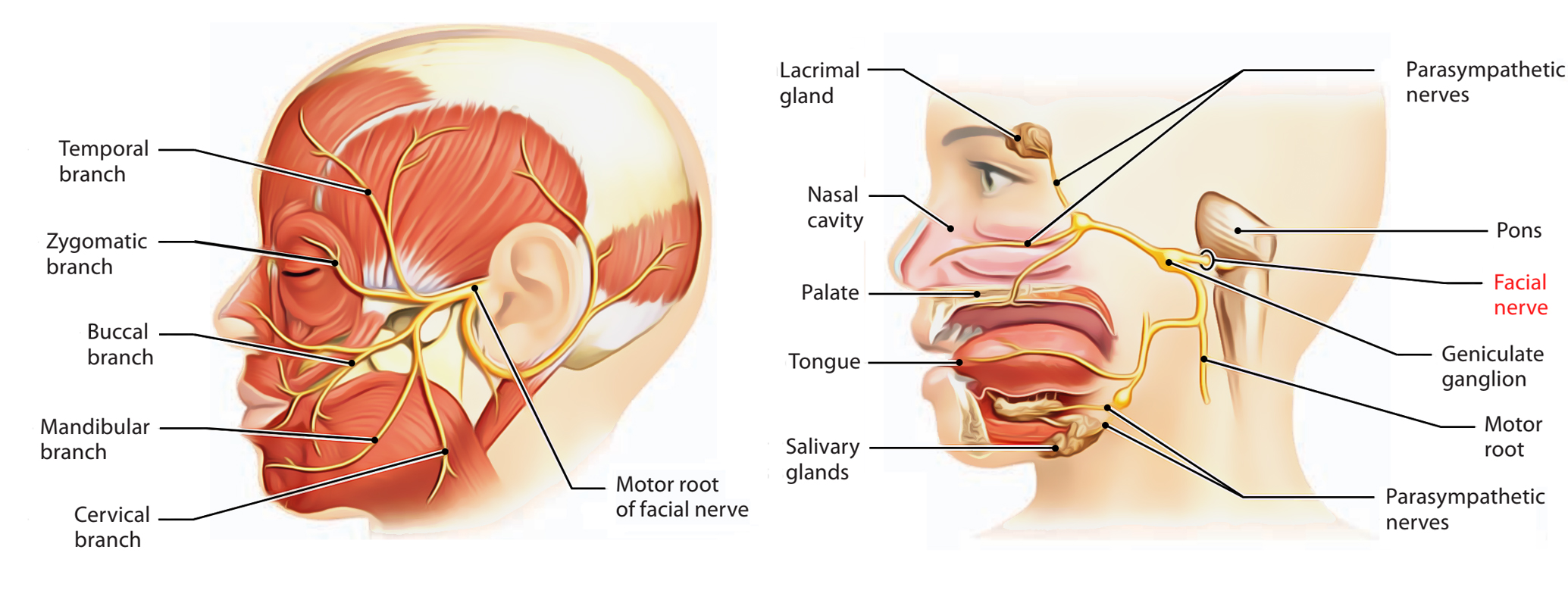
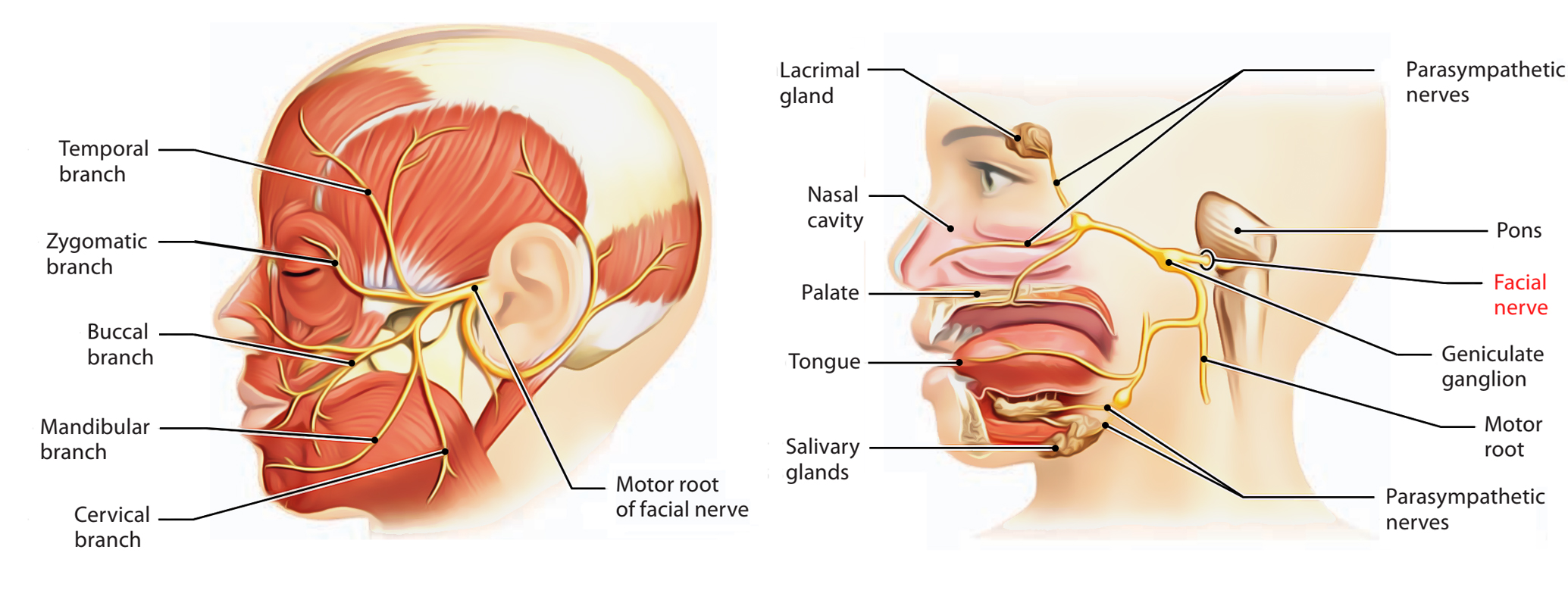
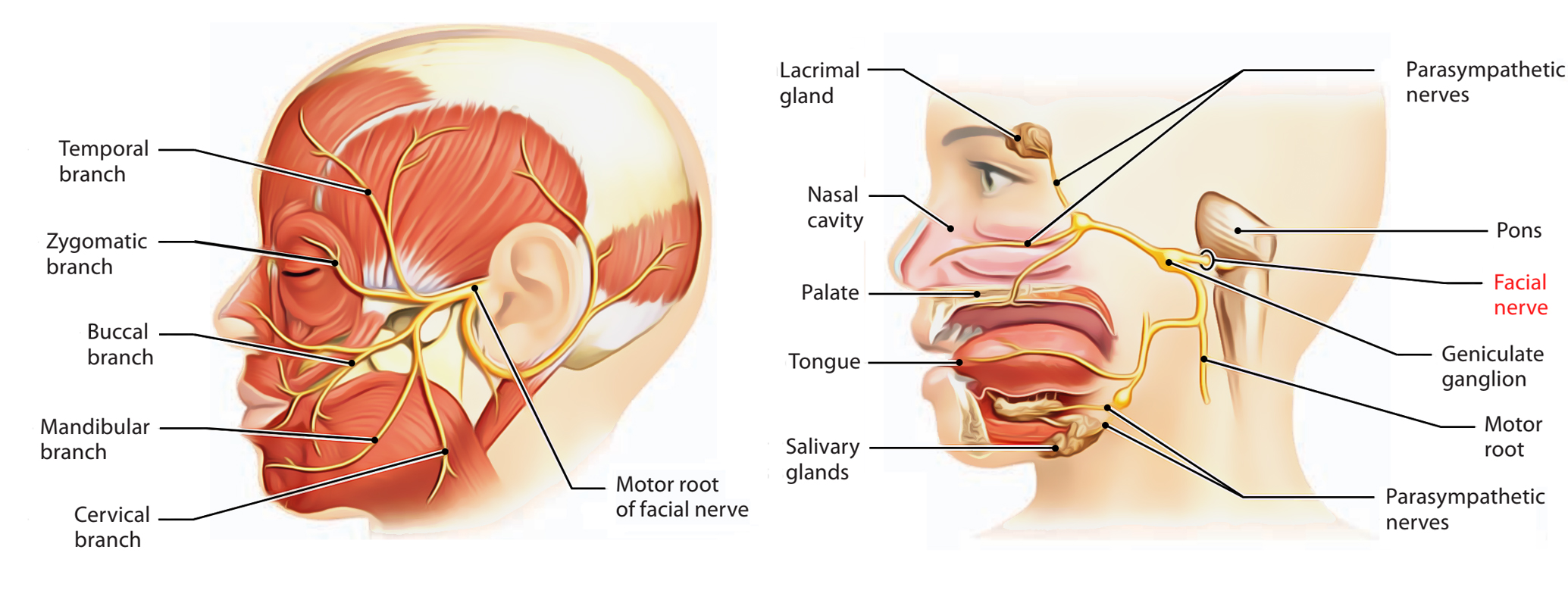
- There is swelling with compression of the nerve in its bony canal.
- It can be due to a varicella zoster inflammatory process and is then called Ramsay Hunt syndrome
- The differential is usually a small pontine stroke
Clinical
- Subtle to severe facial weakness.
- Sometimes the naive can get the sides mixed up - simply ask patient to close both eyes - there is delayed closure on the affected side
- The eye sign is useful as those with UMN weakness rarely have eye closure issues
- There is subacute onset over days/hours of a facial palsy which may be preceded by pain around the ear or behind the ear on the affected side for a few days.
- May involves complete side of face - forehead, eye, dropped corner of mouth.
- Although a motor nerve there may be altered sensation possibly due to involvement of trigeminal sensory fibres but this is not well explained.
- There may be reduced sensation on anterior 2/3rds of the tongue and hyperacusis and decreased tear production.
- Bell's sign shows the eye moves up and out when trying to close eye.
- Pain and vesicles should alert one to Ramsay Hunt syndrome.
- Look for a VI nerve palsy or other long tract or other cranial nerve signs which would isolate the lesion to the pons and suggest a central lesion.
Clinical Questions
- It is not uncommon that clinicians can get confused with mild cases and often misreport the side affected. The patient may even get confused.
- There are a couple of tests that can help to clear up the picture
- Ask patient to smile or show teeth. The angle of the mouth on the affected weakened side will be lower.
- Ask patient to close eyes - the weak side will be slower and incomplete and there may be a positive Bell's sign
- Inspect the patients forehead - there will be noticeably less wrinkles on the affected side
- Rustle fingers over ear - the affected side may be louder
Differential
- Parotid tumours - usually malignant look for any masses or swelling. Suspect if does not improve (most are better in 8-10 weeks) or there is a palpable mass or lymphadenopathy
- Lyme disease(Bilateral LMN VII) History of tick bite, rash, joint pains etc. Consider serum titers (IgM and IgG for Borrelia burgdorferi.
- Sarcoid - Heerfordt's syndrome (LMN VII), BHL etc...
- Guillain-Barré syndrome (Bilateral LMN) tingling toes and fingers
- Cortical Stroke (weak ipsilateral arm/leg/speech/visual signs) and the eye and above are not affected significantly
- Brainstem Stroke: Pontine Lesion: Associated ipsilateral VI nerve palsy, cerebellar signs, contralateral weakness
Investigation
- FBC, U&E, Glucose, ESR, TFTs may be done
- None usually - CT would be unlikely to show a small pontine lesion
- MRI - if stroke a concern. Can show pontine pathology. There can be nerve enhancement with Bell's near the geniculate gangion. Tumours compressing the nerve may be seen.
- Nerve conduction test/EMG: not standard. May be done in the post acute phase to determine extent of injury to the nerve.
Poorer prognosis
- Complete facial palsy with no recovery by three weeks
- Age over 60 years, Severe pain
- Ramsay Hunt syndrome (herpes zoster virus)
- Hypertension, diabetes, pregnancy
- Severe degeneration of the facial nerve shown by electrophysiological testing
|
Management
- General advice: Reassure the person that the prognosis is good: most people with Bell's palsy make a full recovery within 9 months. Advise the person that: It is important to keep the affected eye lubricated. Lubricating eye drops should be used during the day and eye ointment used at night. If the cornea is exposed after attempting to close the eyes they should seek prompt Ophthalmology advice and should patch the eye and tape it closed at bedtime to protect the cornea using microporous tape.
- If within 72 hrs of onset of symptoms then consider Prednisolone 25 mg BD for 10 days, or Prednisolone 60 mg OD for five days and then daily reduction in dose of 10 mg , followed by a taper, for a total of 10 days improves outcome.
- Consider adding Aciclovir PO for 7-10 days if viral cause suspected e.g. Ramsey Hunt syndrome.
- Artificial tears and eye patch may be needed too. There is usually recovery over 3 weeks to 2-6 months.
- Those who fail to recover should be advised to see their own GP and need ENT referral for exclusion of other causes.
Refer
- Any doubt regarding the diagnosis.
- Recurrent Bell's palsy.
- Bilateral Bell's palsy.
- If the cornea remains exposed after attempting to close the eyelid, refer urgently to ophthalmology.
- If the paralysis shows no sign of improvement after 1 month, or there is suspicion of a serious underlying diagnosis (e.g. cholesteatoma, parotid tumour, malignant otitis externa), refer urgently to ENT.
- If there is residual paralysis after 6-9 months, consider referral to a plastic surgeon with a special interest in facial reconstructive surgery.
References