Themes: Hyperacute Care, ICH, Causes
| Mary is an 80 year old lady who developed some altered speech whilst out on a day trip shopping. She was found to have right face, arm and leg weakness and is dysphasic. She has been brought in by paramedics. She complains of a headache. The time of onset was 5.20 pm. She was FAST positive for speech and arm weakness. Her ECG shows AF. The paramedics think she is worse than when they picked her up. She has diabetes and her BM is 8.9. She has a long history of hypertension and the BP is 200/70 mmHg. She has an NIHSS of 15. It is now 6 pm. You attend the stroke call with the specialist nurse. She has no local hospital records as she is away from home. |  |
|---|
1. Do you think this will be an ischaemic or haemorrhagic stroke
The clues for haemorrhage would be the clinical deterioration as bleeding is a dynamic process and can gradually worsen, the history of hypertension and headache. Ischaemic strokes tend to be at their maximum within the first few minutes of onset but there are sometimes exceptions where the onset is more gradual. The AF suggests she might have had a cardioembolic ischaemic stroke. Ischaemic stroke is generally commoner in this population. Patients in AF may also be on anticoagulants.
2. What is the most important test
A non contrast CT head scan is the quickest way to reliably tell if a stroke is ischaemic or haemorrhagic. CT is very sensitive for blood.
3. Click to see the CT scan
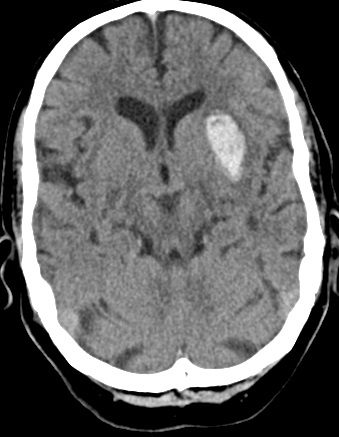
4.Intepret the Scan
The CT below shows a left subcortical haemorrhage. There is minimal oedema and just a tiny amount of midline shift. Haemorrhagic strokes cause 15% of all strokes. It would be good practice to repeat the CT if things got any worse if the patient was someone who might benefit from neurosurgery. It is customary to refer to neurosurgeons though uncomplicated bleeds like this are usually managed conservatively.
5. What actions should you consider
ABC and admission to HASU. Consider ITU if GCS < 9. Check clotting and platelets. The AF concerbs us that the patient may be on Warfarin and a raised INR would suggest this. Try and check the patients medications as they may also be on a DOAC. These would need their specific reversal agent. Stop any Clopidogrel or Aspirin. Monitor and Lowering BP cautiously using local protocols. Monitoring BMs as diabetic. Swallow assessment. Contacting family or those important to the patient to let them know the situation but also to get as much background history as possible and baseline functional status and any views expressed on resuscitation.
6. What are the commonest causes of ICH in this age group
- Chronic hypertension
- Cerebral amyloid angiopathy
- Anticoagulants e.g on warfarin
- Trauma
- Bleeding associated with a tumour
- Arteriovenous Malformation or Cavernoma
7. The INR is 2.2. What actions should you consider
A bedside INR tests shows the INR is 2.2. This would suggest the patient is on Warfarin. The most effective way to reverse the Warfarin is to give Vitamin K 10mg IV and 4 factor Prothrombin complex concentrate such as Beriplex or Octaplex. This usually comes from the blood bank and you will need to call them and explain the urgency. It is very expensive and in some centres you may need to discuss with haematology consultant on call. In some centres it can be ordered by the stroke consultant and this helps to speed up the process. Ensure this is prescribed and administered as soon as possible. Usually in a life threatening bleed the full dose (50 u/kg) is given. You will need to know body weight.
Related Pages
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |