Learning objectives
|
Introduction
- Cognition has been variously defined as the mental action or process of acquiring knowledge and understanding through thought, experience, and the senses. It's basically what the brain does when you peel away all those easily definable actions such as appreciating sensation and motor output and vision. It is what the processing that the brain does between assessing and integrating sensory input and the defining a resultant effector output. Like any computer it requires memory and appropriate processing of input to generate output.
- Poor cognition will prevent you playing chess well but can also prevent you being able to care for yourself or to walk or talk and interact with others. Cognitive impairment is common following stroke. It can significantly affect care and quality of life. There is a high risk of developing dementia within the first year of stroke. Screening and assessment are needed. There are various neuropsychological assessments which can evaluate cognition following stroke. Stroke is often seen in older patients there may already be a baseline cognitive issue. It is important that patients have cognitive assessment. There are a variety of different tests but many of these depend on engagement and patients are often unable to complete tests.
- Cognitive impairments can limit and reduce the success of rehabilitation outcomes and disease prognosis. Persisting defects can cause an inability to work and to take care of one's self and will increase care needs. They can create issues around risk and safety and can complicate discharge planning. Cognitive defects can be seen in patients with additional visual, motor and sensory impairments as well as apraxias and language issues. Stroke affects the cognitive domain, which includes attention, memory, language, and orientation. Affected domains most affected are attention and executive functions. Memory impairment is often prominent.
Affected domains
- Confusion: not orientated in place or time or person. Bizarre behaviours or words or statements. Can easily be confused with dysphasia.
- Attention: those with cognitive impairment are often distractible and cannot focus for long on any particular task
- Memory: inability to learn and recall new information or remember and retrieve long term memory. May be subtle but can affect all aspects of daily living. Can be addressed by establishing a standard daily routine, keeping frequently used items in a designated place, and using a notebook for important information and by supervision if needed.
- Fluency/Language: language may be affected
- Visuospatial: getting lost, lack of orientation. Often seen as a right parietal defect
- Anosognosia: failure to recognise own deficits - a lack of insight into their impairment. Will believe they can walk and deny any deficit which leads to falls. Seen classically with right hemispheric strokes.
- Behavioural issues: impulsiveness, failure to identify risks and does not think of risks before acting. Seen with frontal lobe or non-dominant cortical strokes. Attempts may include trying to drive, cook, walk without assistance or aids. Impulsiveness can also lead to sudden anger, yelling, crying or rude remarks. Needs a familiar safe environment. A regular schedule. Supervision as needed. Remove sharp knives, matches, car keys, etc
- Apraxias: unable to do complex tasks despite normal motor/sensory
- Executive dysfunction: unable to solve problems that require some planning and execution e.g. how to make cup of tea
- Prosopagnosia, also known as "face blindness", is the inability to recognise faces. Lesion is in the occipito-temporal lobes and fusiform gyrus which activates specifically in response to faces. The inferior occipital areas are mainly involved in the early stages of face perception and the anterior temporal structures integrate specific information about the face, voice, and name of a familiar person.
Aetiology
- Ischaemic stroke is a significant risk factor for vascular cognitive impairment and vascular dementia. Studies have shown that in patients with ischaemic strokes that enlarged perivascular spaces are cross-sectionally associated with age, hypertension, and white matter hyperintensities and suggest that enlarged perivascular spaces in the basal ganglia are associated with cognitive impairment after one year.
- Assessment of cognition involves a full assessment of possible defects. These will often become apparent in the first few days after stroke and can be detected by medical and nursing staff as well as therapists who will focus on those which will impair functionality. Cognition and the ability to simply take in and process information will also be impaired by tiredness, pain or depression can all affect your ability to take information in and remain focused.
Cognitive losses and aetiology
| Site/Artery | Cognitive Deficit |
|---|---|
| Left MCA | Aphasia, Mutism, Apraxia, Agraphia, Acalculia, Ideational apraxia, Right/left confusion, C/L face/arm/leg weakness and Sensory loss |
| Right MCA | Neglect, Visuospatial losses, Loss of prosody, Anosognosia, C/L face/arm/leg weakness and Sensory loss |
| Posterior cerebral artery | Colour agnosia, Associative visual agnosia, Alexia (hemianopic and pure), Facial agnosia, Bálint’s syndrome, Amnesia |
| Anterior cerebral artery | Deficits in planning, initiation, monitoring, concentration, and flexibility, C/L leg weakness and Sensory loss |
| Deep Subcortical/Thalamic | Reduced arousal, attention, motivation, initiation, and executive function, Memory (verbal, visual, episodic declarative, anterograde, and retrograde) |
| Caudate | Impaired problem solving and attention, Memory |
| SAH due to A comm Aneurysm | Amnesia, Personality changes, Confabulation, Abulia due to damage to the mesial frontal cortex |
| Limbic and paralimbic lesion | Difficulties in learning and retaining new information, Affective changes |
Memory
| Types of memory system | Meaning | Location |
|---|---|---|
| Long term memory | episodic memory, semantic memory, autobiographical memory, procedural memory. | Medial temporal lobe, diencephalon |
| Semantic memory | Structured record of facts, meanings, concepts and knowledge about the external world that we have acquired | Inferior and lateral temporal lobe |
| Episodic memory | Memory of experiences and specific events in time in a serial form. Memory of autobiographical events (times, places, associated emotions and other contextual knowledge) that can be explicitly stated. | Medial temporal lobe, diencephalon |
| Procedural memory | Long-term memory responsible for knowing how to do things, also known as motor skills. | Basal ganglia, cerebellum |
| Short-term memory | Working memory | Prefrontal cortex |
Balint's syndrome
An acquired disturbance of the ability to perceive the visual field as a whole due to bilateral parietal-occipital damage from strokes or Alzheimer disease, and traditionally, is considered to include three components
- (1) ‘visual disorientation’ (also known as ‘simultanagnosia’)
- (2) ‘ocular apraxia’ (also known as ‘psychic gaze paralysis’)
- (3) ‘optic ataxia.’
The key constituent in the syndrome, however, is visual disorientation.
Prosopagnosia
Prosopagnosia, also called face blindness, is a cognitive disorder of face perception in which the ability to recognize familiar faces, including one's own face (self-recognition), is impaired, while other aspects of visual processing (e.g., object discrimination) and intellectual functioning (e.g., decision-making) remain intact.
Anton's syndrome
Anton–Babinski syndrome, also known as visual anosognosia, is a rare symptom of brain damage occurring in the occipital lobe. Those who have it are cortically blind, but affirm, often quite adamantly and in the face of clear evidence of their blindness such as walking into objects, that they are capable of seeing. This increases the risks of harm and injury and patients need close supervision.
Cognitive Tests
- Folstein's mini-mental state examination (MMSE): Cognitive impairment after stroke has been defined as a mini mental state examination score of less than 26, recorded at one-year post stroke.
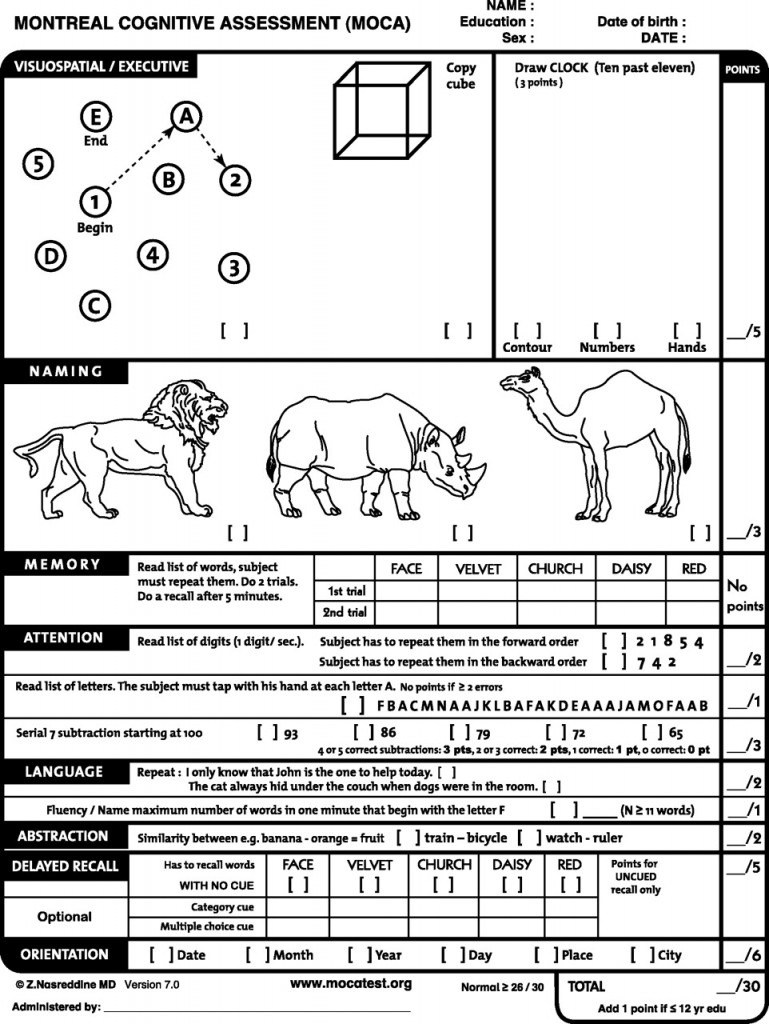
- Montreal cognitive assessment (MoCA)
- Addenbrooke's cognitive examination (ACE-III)
MMSE
The MMSE should be used as a screening device for cognitive impairment in which a low score indicates the need for further evaluation. It should not serve as the sole criterion for diagnosing dementia or to differentiate between various forms of dementia. The MMSE scores may be used to classify the severity of cognitive impairment or to document serial change in dementia patients. The test assumes fluency in English. A lower score may be seen in those with low educational attainment. It also assumes that patients are doing their best, are not fatigued and low mood can affect it and so it may needed to be repeated at intervals.
- No cognitive impairment=24-30
- Mild cognitive impairment=18-23
- Severe cognitive impairment=0-17.
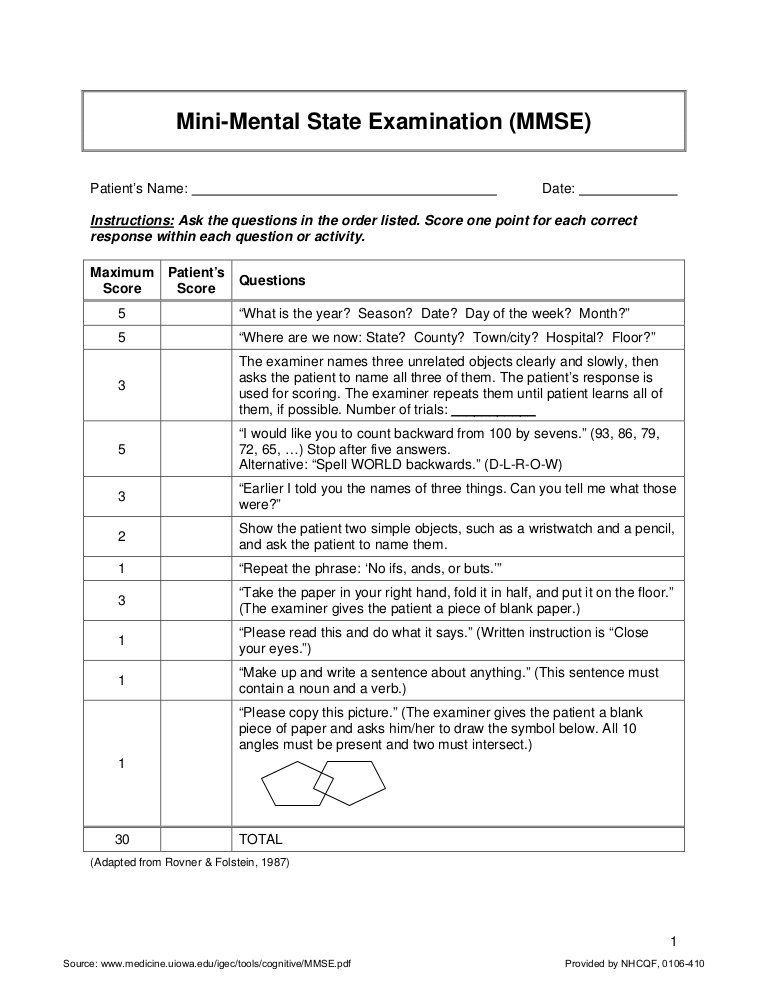
MMSE
ADDENBROOKE’S COGNITIVE EXAMINATION – ACE-III
References and further reading
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |