Learning objectives
- The importance of cardioembolic stroke
- Detection of causes of cardioembolic stroke
- General Management of cardioembolic stroke
|
Introduction
- This refers to strokes due to emboli arising from the heart.
- Either from the left atrium, left ventricle or valves or via a shunt such as a PFO or ASD.
- Cardioembolic stroke accounts for between 15-30% of all acute ischaemic strokes.
- In-hospital mortality in cardioembolic stroke is high at 25-30%
- Over 20% of strokes in the over 80s are due to AF which are potentially preventable
Causes
| Causes of Cardioembolism |
|---|
- Highest risk
- Atrial fibrillation risk depending on CHADS-VASC score
- Recent MI (LV aneurysm/hypokinetic and akinetic ventricular walls)
- Mechanical heart valve
- Dilated cardiomyopathy
- Mitral rheumatic stenosis
- Post Cardiac Surgery e.g. Valve replacement or TAVI or PCI
- Rheumatic heart disease
- Left atrial appendage thrombus
- Atrial Myxoma
- Infective Endocarditis
- Libman sacks endocarditis
- Mitral papillary fibroelastomas
- Atrial septal defects
- Patent foramen ovale and atrial septal aneurysms
|
Classification
- Cardiac wall and chamber abnormalities
- Cardiomyopathies
- Hypokinetic and akinetic ventricular regions after myocardial infarction
- Atrial septal aneurysms
- Ventricular aneurysms
- Atrial myxomas
- Papillary fibroelastomas
- Septal defects and patent foramen ovale
- Valve disorders
- Rheumatic mitral and aortic valve disease
- Prosthetic valves
- Bacterial endocarditis
- Fibrous and fibrinous endocardial lesions
- Mitral valve prolapse and mitral annulus calcification
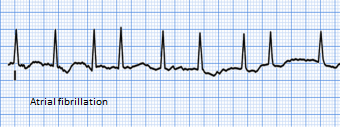
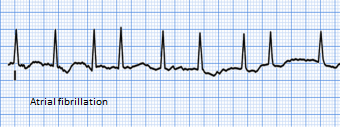
- Arrhythmias
- Atrial fibrillation
- "Sick-sinus" syndrome.
Clinical
- Embolic strokes tend to be acute and maximal at onset.
- They may be preceded by a cough or sneeze or a valsalva
- Can suddenly improve due to passage of the clot distally, variability in collaterals and spontaneous reperfusion.
- There is often a large vessel obstruction amenable to thrombolysis and thrombectomy.
- There is a greater risk of haemorrhagic transformation.
- Multiple stereotypical clinical syndromes in the same territory is not cardioembolic source.
- One caveat is that it can be hard to differentiate cardioembolism from embolism from aortic arch plaque
Causes and Frequency
| Site | Frequency | Risks | |
|---|
| Non Valvular AF | 50% | AF has a 3 to 5 fold increased risk of stroke. Assess using CHADS-VASC score and consider NOAC/Warfarin |
| Acute MI | 10% | 2.5% of patients experienced a stroke within 4 weeks of acute MI |
| Ventricular thrombus | 10% | Mural thrombus may be seen post MI |
| Rheumatic heart disease | 10% | Rheumatic Mitral stenosis particularly high risk ( x 17 fold increase) and needs warfarin and not a NOAC |
| Prosthetic Metal valves | 5% | Needs Warfarin. No role for DOAC |
| Others | 15% | |
| A dense artery may be seen with a large embolic thrombus | Atrial Fibrillation | large STEMI |
|---|
 |  |  |
| Cardioembolic infarction is generally the most severe ischaemic stroke subtype, with a low frequency of symptom-free at hospital discharge, a high risk of early and late embolic recurrences, and a high mortality |
| A list of Aetiologies for Cardioembolic Stroke stroke |
|---|
|
|
| Characteristics |
|---|
- Acute onset to maximal severity instant
- Multiple territory
- Non stereotypical neurology
- Large vessel usually but showers of small embolic can occur
- Decreased level of consciousness at onset
- Haemorrhagic transformation of an ischaemic infarct
- Early recanalization of an occluded intracranial vessel
|
Structural Cardiac disease and stroke
Various Cardiac structural defects can lead to the formation of intracardiac thrombi and cardioembolism. If suspected the first investigations include a clinical history and a search for any determinants that will give a clue. Cardiac symptoms suggestive of ischaemic heart disease, chest pain, breathlessness and palpitations which could suggest an ischaemic cardiomyopathy. A history of rheumatic fever could suggest valvular disease. A history of excess alcohol might suggest an alcoholic cardiomyopathy. Cardiomyopathy may also be seen with HIV. Examination may reveal heart failure, rashes, AF, sighs of chronic liver disease, nicotine staining, hypertension and murmurs. An ECG, CXR and then Echo will be useful. A troponin may be useful acutely if recent myocardial infarction is suspected. Temperature and stigmata for endocarditis must always be considered. Most embolism is thrombotic but other rare sources of emboli are air, fat, cholesterol, bacteria, tumour cells, and particulate matter from injected drugs should be considered in rare cases.
| Cause | Details |
|---|
| Severely Impaired LV function | Impaired LV function ( < 20%) when severe can be a risk factor for embolism and an annual incidence of about 3.5% has been quoted with chronic heart failure but these patients often have associated AF which adds to risk. Patients need an Echocardiogram. For those with AF a related scoring should be done. For those without AF then an individualised assessment of risk and benefits of anticoagulation should be assessed as well as optimising heart failure management and treating any cause. |
| Infective endocarditis | Endocarditis has a high risk of embolism especially in the first 7-10 days. Haemorrhagic changes are often seen and anticoagulation avoided acutely. |
| Marantic endocarditis | Cancer and stroke. Cancer can cause a hypercoagulable state. |
| Atrial myxoma | A cause of fever, raised ESR and cardioembolic stroke |
| Myocarditis | Often viral infection with malaise, heart failure, arrhythmias |
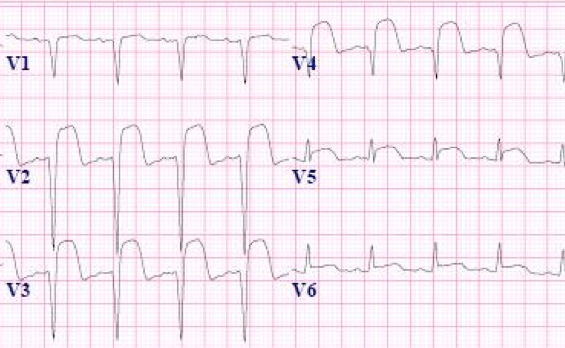
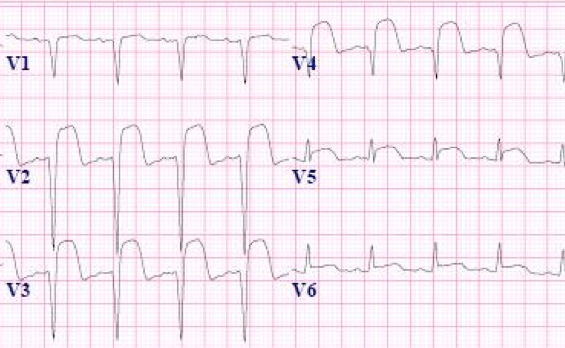
| LV aneurysm | Usually seen following Large anterior STEMI. May be LBBB or persisting ST elevation on ECG |
| Cardiomyopathy | Diseases affecting heart muscle. |
| Mitral Valve Prolapse | Studies have shown that mitral valve prolapse (MVP) is associated with fibrinous deposits on the valve, endothelial denudation and annular thrombus at the junction with the atrial wall. The myxomatous redundant valve leaflets appear to increase the predisposition to thromboembolic events. There is no evidence for antithrombotic treatment other than antiplatelets in those who have experienced stroke. There should be a search for undetected PAF. | |
| Mitral annulus calcification | Is seen with mitral stenosis, mitral regurgitation and may be increased in those with cardiogenic brain embolism. Detected on echocardiography it suggests a twofold increase in risk for stroke. Embolism of fibrinated cell clot or calcium spicules has been reported. | |
| Patent foramen ovale + DVT | Patent Foramen Ovale |
| Prosthetic Heart Valves | Diseased and damaged heart valves are often replaced with either mechanical or bioprosthetic (tissue) valves. Tissue prosthetic valves are believed to be associated with a smaller risk of thromboembolism than mechanical valves. Mitral valve prostheses are associated with a greater risk of thromboembolism than Aortic, possibly because of the higher incidence of atrial fibrillation and other thromboembolic risk factors in these patients. | |
Clinical
- Sudden onset of an acute arterial syndrome
- Most often MCA, then PCA, ACA or Vertebral/PICA or Basilar
- May be AF on examination. Murmurs, Clubbing (myxoma)
- Signs of endocarditis
- Recent chest pain or breathlessness from an MI
Investigations
- FBC and ESR: elevated ESR with atrial myxomas and endocarditis or malignancy
- ECG: may show recent STEMI with Q waves or persistent ST elevation suggesting ventricular aneurysms. It may also show AF or sick sinus syndrome.
- Detect AF: 24-48 hour Holter monitoring or even 7 day which may be repeated
- Implantable loop recorder : placed subcutaneously. Can be interrogated about recent rhythms
- CXR: may show an enlarged heart
- CT Scan: multiple territory infarcts
- CTA: May be large vessel obstruction seen on CTA from a large thrombus from the heart
- MRI: May show a large vessel stroke or occasionally an embolic shower with multiple pinpoint infarcts seen on DWI/ADC map
- Transthoracic Echo: Assess LV function, valves and myocardium
- Bubble echo: useful to identify right to left shunt causing a paradoxical embolism
- Transoesophageal echo: Helps to visualise vegetations on valves, PFO, atrial myxoma also aortic arch and ascending aorta, left atrium and left atrial appendages, intra-arterial septum, pulmonary veins
- Transcranial doppler : bubble tests can help identify shunting
Management
- Standard Ischaemic stroke Management. Treat cause.
- Secondary prevention with anticoagulants should be started as per guidelines usually at 1-2 weeks on a case based approach. Caution in endocarditis.
References