Learning objectives
|
Introduction
- Acute basilar artery occlusions are rare, accounting for approximately 1% of strokes
- Presentation can be subtle and difficult to diagnose without some focal neurological clues
- A spectrum of symptoms and outcomes usually with some degree of posterior circulation damage
- It can be progressive with devastating consequences
Anatomy
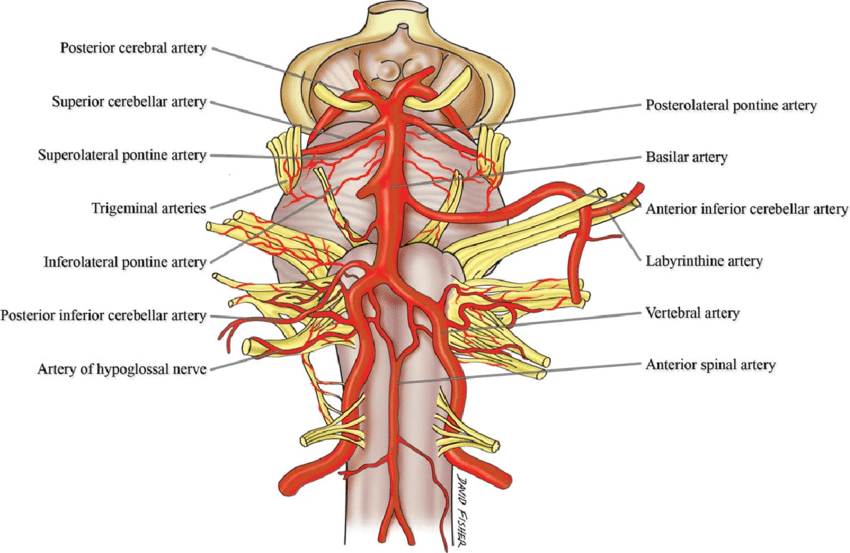
- The basilar artery is formed by the fusion of the vertebral arteries commencing at lower pons.
- The artery ascends in what is called the basilar sulcus in front of the pons
- Divides at upper pons / midbrain junction into Right and left PCA
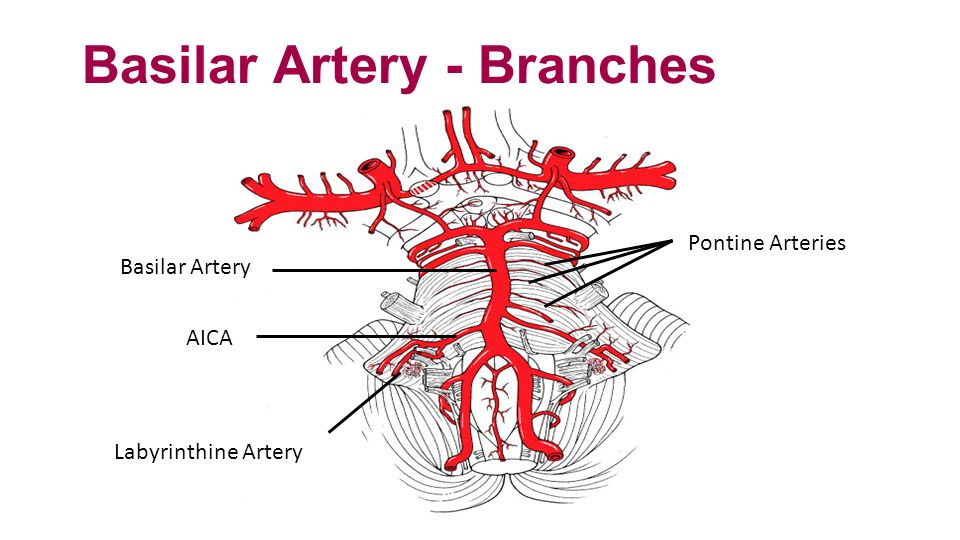
Branches of the Artery
- Anterior inferior cerebellar artery (AICA)
- Labyrinthine artery (variable origin; more commonly a branch of AICA)
- Pontine arteries: origin occluded can cause unilateral or bilateral ventral pontine infarcts
- Superior cerebellar artery (SCA) infarcts upper cerebellum and lateral pons
- Posterior cerebral arteries : Infarcts occipital cortex + part of midbrain and thalamus
Aetiology
- The artery supplies the midbrain, the thalamus, and the medial aspect of the temporal and the occipital lobes.
- Occlusion of the basilar may be due to cardioembolism, artery to artery embolism or thrombus in situ from localised disease.
- Consider vertebral artery dissection or vertebral/basilar/subclavian atherosclerosis
- Often the occlusion can be staggered with a slow accumulation of clot and then total catastrophic obstruction.
Causes
- Atrial fibrillation and other causes of cardioembolism
- Cervical dissection
- Cocaine usage
- Subclavian/Vertebral/Basilar atherosclerosis
- Arteritis, meningitis, aneurysms
- Hereditary arteriopathies
- Neurosyphilis, Behcet vasculitis
Imaging
| Hyperdense basilar artery (HDBA | Posterior circulation infarction | Posterior circulation infarction |
|---|---|---|
 |
 |
 |
Clinical
- Rarely can be subtle posterior circulation events
- Usually sudden collapse and comatose
- Quadriparesis, Diplopia, Cerebellar ataxia
- Pinpoint pupils with pontine infarction
- Lateralising Sensory/Motor signs and ipsilateral cranial nerve palsy
- Amnestic type symptoms
- Locked in syndrome
Investigations
- FBC, U&E, LFTs, Glucose, Lipids, CRP
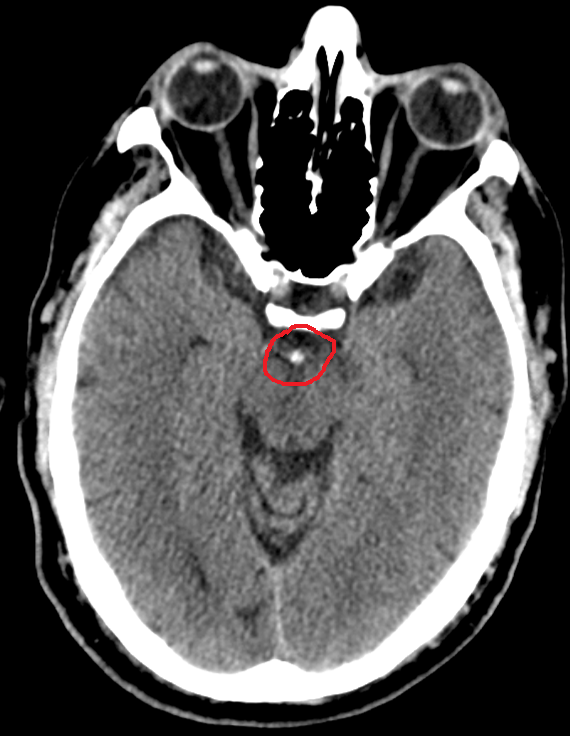
- CT:When diagnosis suspect a CT is needed which may show a hyperdense basilar artery in about 70-80%
- CTA: More useful and if basilar occluded then is needed for thrombectomy and may show causes e.g. vertebral dissection. Successful recanalization appears to be the single most important predictor of a good outcome. The presence of bilateral PCOMs on pretreatment CTA appears to be associated with more favorable outcomes in BAO treated with Endovascular therapy. The primary collateral pathway of the posterior circulation from the anterior circulation occurs via the posterior communicating arteries.
- MRI can be done later and will show extent of damage and restricted diffusion within infarcted tissue
- ECG: ? AF
- Echo : source of embolism
Poor prognostic indicators
- Age, Current smoking, Hyperlipidemia
- Time to treatment
- Intubation at 24 to 48 hours
- Intubation at initial presentation
- History of minor stroke
- Baseline NIHSS
- 24- to 48-hour NIHSS
- BATMAN score < 7
Favourable Prognostic Indicators
- Successful recanalisation
- Bilateral PCOMs on pretreatment CTA
- NIHSS ≤4 at 24 to 48 hours
BATMAN Score at CTA
- Flow in Both vertebral arteries + 1(considered as 1 segment)
- Flow in Proximal segment of the basilar artery + 1
- Flow Middle segment of the basilar artery +1
- Flow Distal segment of the basilar artery +1
- Flow P-1 segment of the PCA +1
- Filling of each PCOM +2
- Filling in a hypoplastic PCOM +1
- A score of 10 suggests normal arterial filling of the posterior circulation and a score of 0 suggests no filling of the posterior circulation. In their multivariate analysis, an unfavorable BATMAN score (defined as < 7) was independently associated with poor outcome (defined as an mRS of 4 or greater)
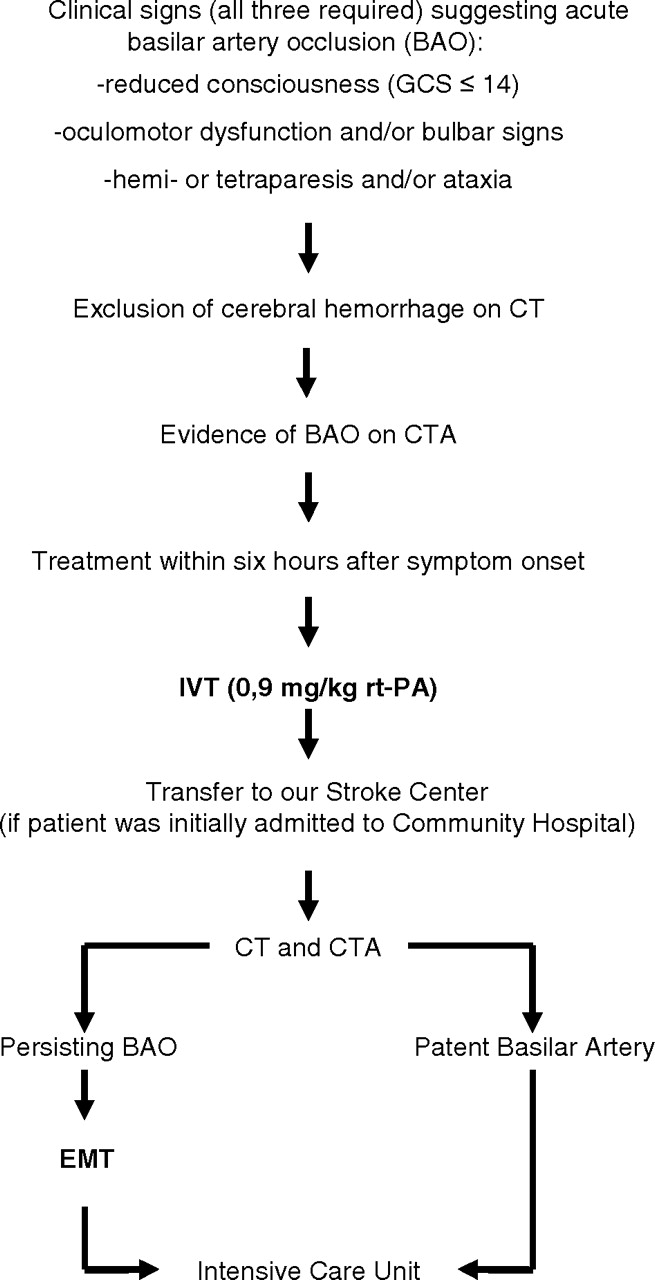
Suggested Algorithm (Follow your local guidance) from References
Management
- ABC and resuscitation, May need intubated and ventilated acutely. Often an ITU bed is needed acutely with close management of airway due to bulbar weakness.
- Discussion immediately with local thrombectomy centre usually following local CTA and then immediate transfer to interventional radiologists.
- At this stage thrombolysis should be considered for those certainly within the 4.5 hrs window or even out to 6 hours on a case by case assessment.
- Emergent IV/IA Thrombolysis and Mechanical Thrombectomy is treatment of choice even with thrombectomy up to 12 or even some quote 48 hours especially if there is a small core with a high NIHSS score.
- NIHSS ≤4 at 24 to 48 hours is highly associated with a favourable outcome at 1 month, whereas an NIHSS≥28 universally portends a poor outcome.
- Prognosis however is often grave and survival may be with significant disability including locked in syndromes
- Palliation and end of life care may be appropriate in those with very poor prognosis
References
- Basilar Occlusion Syndromes: An Update. The Neurohospitalist 2015, Vol. 5(3) 142-150
- Basilar artery occlusion. Lancet Volume 10, No. 11, p1002–1014, November 2011
- Rangaraju S et al. Neurologic Examination at 24 to 48 Hours Predicts Functional Outcomes in Basilar Artery Occlusion Stroke. Stroke. 2016;47:2534-2540
- Posterior circulation CT angiography collaterals predict outcome of endovascular acute ischemic stroke therapy for basilar artery occlusion. J Neurointerv Surg. 2016 Aug;8(8):783-6.
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |