Learning objectives
|
Status:Major rewrite
| Axial cross section shows the orientation of the skull facing down and imaging such as MR and CT show the skull looking up. It makes more sense to get use to the radiological presentation of anatomy. |
Introduction
It is important to develop a good three dimensional knowledge of brain anatomy to aid the correlation between imaging related changes and the expected functional aspects expected in terms of clinical signs and vascular supply. Knowing the anatomy and shape of the lesion can also help explain aetiology. You need to develop an appreciation of what is also normal anatomy and the variations. Although we mostly use axial imaging it is important to look at coronal and sagittal sections. Once we know the parenchymal anatomy we need to know the vascular supply. Stroke is set of different clinical syndromes due to the location of the vascular pathology. Location and appearance can help to pinpoint the likely aetiology.
There are many beautifully illustrated textbooks of neuroanatomy available and it is important that you get one but here I am going to try and keep illustrations to keep ideas simple and concepts easy to follow. You need to basically know pathways, relationships and vascular supply. Most of the books I recommend are so beautifully illustrated that your eyes and visual cortex are quickly overloaded and the simple concepts are easily lost in an ocean of detail. Learn the basics schematic type concepts first and then these detailed diagrams will mean much more to you. So I make no apologies for my hand drawn and scanned images below and on other pages. There is I feel often a delight in the detail by those neuro-anatomists who fail to communicate basic and easily memorable common themes. I have tried to make the anatomy memorable, it is. If you can navigate yourself around you local neighbourhood then you can do neuroanatomy.
Names are basically of Greek and some Latin origins. There is some terminology to learn. This is unavoidable. Do not be put off. There will be lots of repetition like learning a new language and if you stick with it you will do fine.
The Nervous system
The nervous system is divided into the central and peripheral systems. It is only the central nervous system that concerns us with stroke.
|
Embryology:
This is the part most people skip but there are some general memorable terms and structural concepts. Come back to this later on when you are comfortable with the terminology and have a basic idea how the structure is of the CNS. There are different terms used and I want to keep this as simple as possible but you may well come across it in the bigger neuroanatomy books.
|
General overview
The cerebral cortex is divided by the falx into two separate right and left cerebral hemispheres but connected by the corpus callosum. The surface markings and groves called sulci mark the brain into four lobes. They have distinctive roles. In general the brain and most particularly the cerebrum acts as a processor. The input is sensory and the output motor.
- Sensory input comes into the body as touch, smell, vision, hearing, language and is integrated and a certain conscious motor response is generated that is then communicated to the corresponding muscles. All of sensation below the neck comes via the spinal cord and its 31 nerves and the cranial nerves that have a sensory role. Sensation in the face comes via the trigeminal nerves. All of this ends up in the contralateral parietal lobe for processing. It all travels via spinal nerves and though the spinal cord and brainstem to the thalamus and then to the parietal lobe.
- Conscious motor out begins in the prefrontal gyrus of the lobe where it has its cell body and travels as a corticospinal axon down through the corona radiata into the posterior limb of the internal capsule and into the cerebral peduncle and through descending fibres in the pons and then on the pyramids of the medulla where they decussate (cross sides) and into the spinal cord where it synapses with the anterior horn cell and exits at the corresponsing level to the brachial or sacral plexus to move the arm or the leg. Cortibulbar fibres also descend similarly but they exit the shared path in the brainstem and exit to cause facial expression (facial nerve) or speech or tongue movement (hypoglossal) or mastication (trigeminal).
Cerebral Dominance
An examination of the two cerebral hemispheres shows that the cortical gyri and fissures are almost identical. Nerve pathways projecting to the cortex do so largely contralaterally and equally to identical cortical areas. The cerebral commissures and corpus callosum and the anterior commissure allow information that is received in one hemisphere to be transferred to the other. Despie this symmetry and free movement of information certain nervous activity is predominantly performed by one of the two cerebral hemispheres. Handedness, perception of language, and speech are functional areas of behavior that in most individuals are controlled by the dominant hemisphere. By contrast, spatial perception, recognition of faces, and music are interpreted by the nondominant hemisphere. Generaly a right handed person has a dominant left hemisphere. 50% of left handers have a dominant left hemisphere.
Lobar Anatomy
The Cerebral cortex is the most developed part of the human brain. The surface is the processing centre comprised of the outer layer of grey matter formed by neuronal cell bodies. These are connected with neighbouring areas by wire like axons which are myelinated and pass to other cortical areas or as long tracts to other nuclei or pass down to the brainstem and spinal cord. These fibres contain both ascending (mainly sensory) and descending signals (mainly motor). Others form circuits within the deep grey matter of the basal ganglia and other structure grey matter structures such as the thalamus. Some pass to the opposite cortex through the corpus callosum. The hemispheres surround the fluid filled ventricles.
There are two cerebral hemispheres separated by a longitudinal fissure and a stiff membrane called the falx cerebri. The hemispheres are connected by the corpus callosum. Each cerebral hemisphere can be divided by certain sulci on the brain surface into lobes. The surface shows multiple folds - gyri (the hills) and sulci (the valleys) which increase the amount of grey matter. It was Broca, a french scientist who showed that different parts of the brain had distinct functions. He did this by showing that in the subsequent post mortem of a patient who while alive had had a speech disorder - dysphasia had a lesion in the precentral gyrus later called Broca's area. Later others such as Brodmann mapped these areas on their cellular appearance.
Anatomy and Function
| Lobe and other structures | Basic Function |
|---|---|
| Frontal Lobe | Producing Movement to the other side of body - eyes, face, arm, leg, Producing language (Dominant), Decision making, Behaviour |
| Parietal Lobe | Sensation of other side of body, Interpreting speech, Vision to the opposite side (inferior quadrant) |
| Temporal Lobe | Memory, Interpreting speech, Vision to the opposite side (superior quadrant) |
| Occipital Lobe | Vision to the opposite side |
| Thalamus | Integrates and relays sensory information to the cortex of the parietal, temporal, and occipital lobes from the opposite side. |
| Basal ganglia | Help to coordinate movement |
| Cerebellum | Coordination on the same side |
| Midbrain | Nerves that move the eye, movement to the other side, sensory |
| Pons | Nerves that move the eye, mastication, sensory face, facial expression, movement to the other side |
| Medulla | Swallowing, balance, tongue, breathing, heart rate, blood pressure, movement to the other/same side |
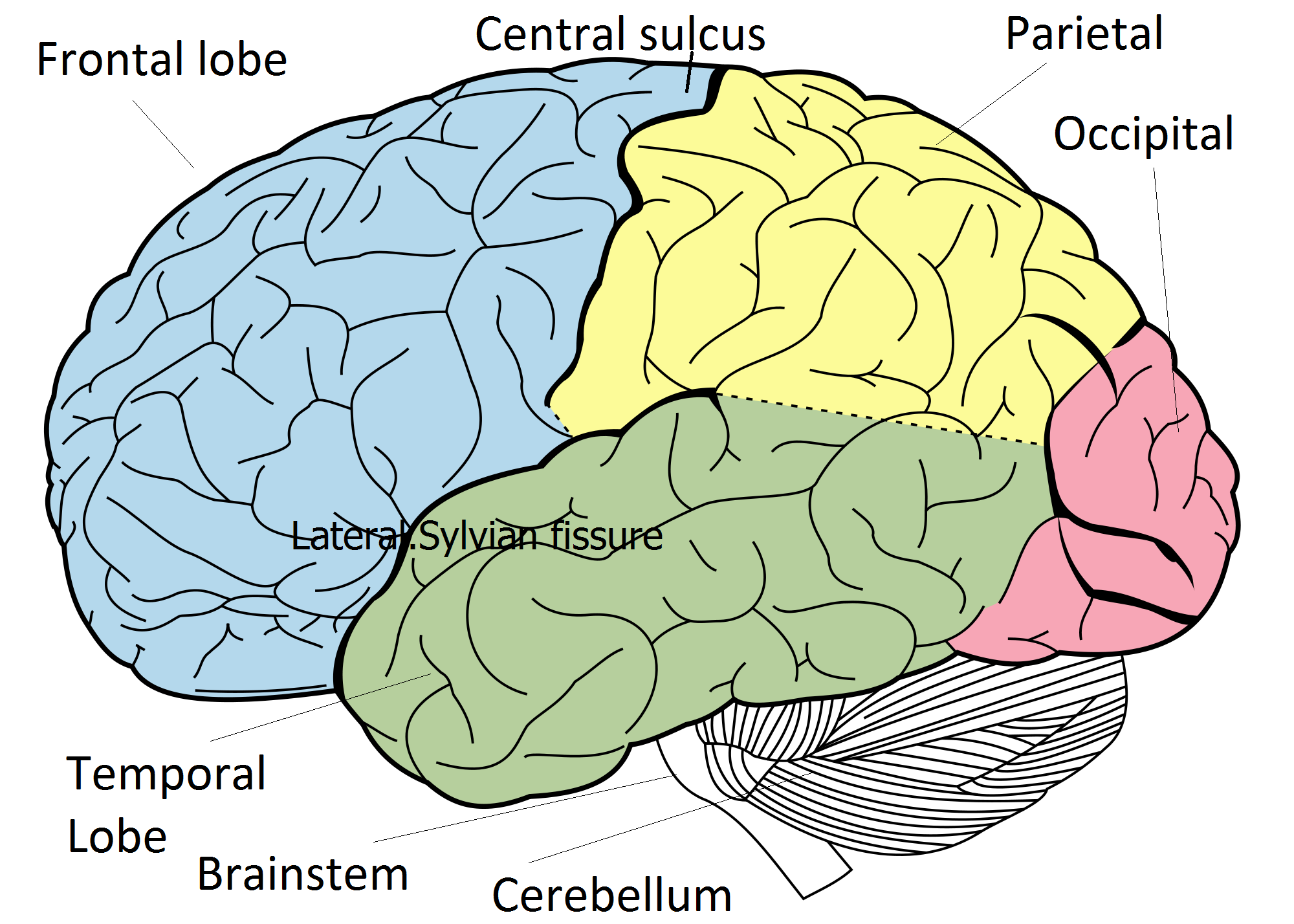
Important surface sulci to identify
- Central sulcus: separates frontal and parietal lobes where the primary motor cortex and primary sensory cortex like closely together
- Lateral/Sylvian sulcus (fissure) forms the upper limit of the temporal lobe
Frontal lobe: Motor/Eye movements/Language/Executive
The frontal lobe lies in front of the central sulcus. Below it is limited by the lateral (sylvian) sulcus. It contains the primary motor cortex (MC) which lies on the pre-central gyrus. The frontal lobe gets input from the thalamus and cerebellum. It is source of all conscious movement. Representation on the lateral surface is hand superiorly and then below that face and tongue and larynx and pharynx. The trunk and leg are represented on the medial inner surface. The Premotor cortex (PMC) lies slightly anterior to MC and is also concerned with voluntary movement. The Frontal eye fields lie in front of the PMC and are involved in eye movement. Broca's area (dominant hemisphere) lies inferiorly close to the motor areas for mouth, oral cavity and pharynx and larynx. Broca's is involved in generating the language content of speech. Damage here causes an expressive dysphasia. The lobe is also involved in executive decisons, personality and intellectual ability. The medial aspect (paracentral lobule) is involved with urinary continence.
Parietal lobe: Sensory/Vision/Language
The parietal lobe lies behind the central sulcus and extends as far back as the limit of the sylvian (lateral) sulcus and the parietoccipital sulcus. It contains the Primary sensory cortex on the post central gyrus with representation of hand and face laterally and leg on the inner superior medial section. Areas of high sensory input such as face and hand are given proportionally large representations. All conscious sensation is perceived here. Parietal association cortex mostly involved with integration of sensory input and processing. Input mainly from the thalamus. Deep fibres carry the optic radiations from lateral geniculate ganglion from the superior retina
Temporal lobe: Hearing/Vision/Language/Memory
Temporal lobe lies below the sylvian (lateral) fissure as far back as a line dropped from the end of the sylvian fissure. It contains the Auditory cortex lies in the superior temporal gyrus on lateral surface and is concerned with input from medial geniculate body. Temporal association cortex integrates auditory stimulus and language comprehension (dominant hemisphere) Damage here can cause a receptive dysphasia. Memory processing and recall. Deep fibres carry the optic radiations from the lateral geniculate body from the lower retina
Occipital lobe: Vision
The occipital lobe lies behind the parietal and temporal lobes. It is the Calcarine cortex that primarily deals with vision and visual processing. The optic radiations pass back from the lateral geniculate body of the ipsilateral thalamus. Sight from the right side of ones world goes to left occipital cortex. Occipital association areas concerned with image processing. There is a high density of neurons. The main centre for processing is within the calcarine sulcus. Upper fibres from the upper retina pass to the upper calcarine sulcus called the cuneus. Lower fibres pass to the lower part of the sulcus, the lingual gyrus from the lower retina. The visual area is called Brodmann 17 area.
Insular cortex
This is not a lobe but an interesting part of the brain grey matter which is seen if one parts the lips of the lateral sulcus and is known as the insula. It is closely associated with the middle cerebral artery which passes on the surface. Its functions are poorly understood and possibly involve belching, salivation, gastric movements and vomiting. It may play a role in addiction. The insula certainly is discussed in early stroke imaging 'loss of the insular ribbon sign'.
Cerebral Architecture and Histology
Cerebral Architecture
Histologically the cerebral cortex is made up of a half centimeters of grey cells above a dense thick inner layer of white matter. The overall surface area is increased by the folds of sulci and gyri. The cortex can be seen to be composed of six layers of cells which vary in size and structure. Back in 1909 Brodmann produced a map of the cerebral cortex based on the micro-architecture of the cells and staining for Nissl substance which separates neurons from glial cells. This was before we had understanding of many of the functions of these areas and the system has stood the test of time. Other improvements have been developed by others. It is quite clear that anatomy is related to function.
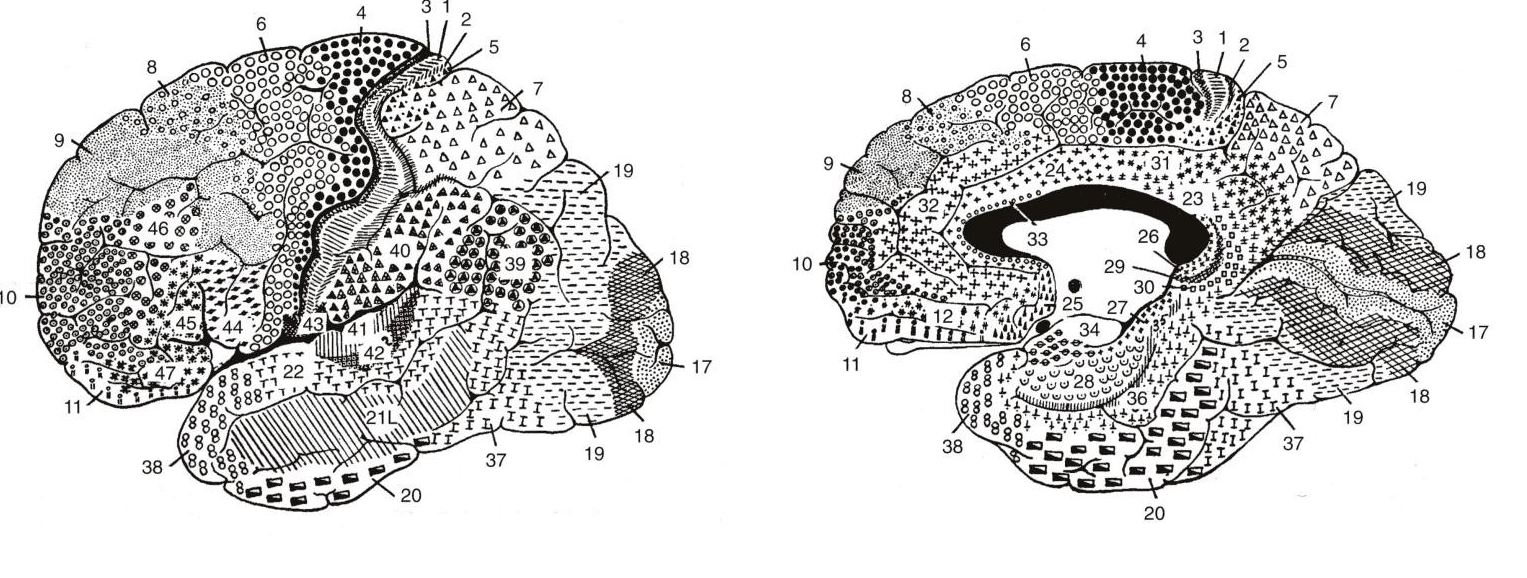 Cells in the cortex are arranged in a columnar structure and can this can be seen with microelectrode stimulation. Areas with similar function lie close together. For example Broca's area lies within the inferior region of the precentral motor cortex near to those areas that control voluntary movement of the lips, tongue, larynx and pharynx. Broca's produces the content of speech content and damage here leads to an expressive dysphasia. A lesion in the inferior area of the precentral motor cortex leads to dysarthria and facial weakness. Broca's discovery of dysphasia in a patient whose subsequent post mortem revealed a lesion due to syphilis in the area that became known as Broca's area was one of the key finding to suggest localization of function within the brain. The fibres from the cortex on their way to the brainstem pass down in a fan like bundle called the corona radiata to enter the internal capsule. Note that neuroanatomical diagrams are "upside down" compared with the normal appearance of imaging
Cells in the cortex are arranged in a columnar structure and can this can be seen with microelectrode stimulation. Areas with similar function lie close together. For example Broca's area lies within the inferior region of the precentral motor cortex near to those areas that control voluntary movement of the lips, tongue, larynx and pharynx. Broca's produces the content of speech content and damage here leads to an expressive dysphasia. A lesion in the inferior area of the precentral motor cortex leads to dysarthria and facial weakness. Broca's discovery of dysphasia in a patient whose subsequent post mortem revealed a lesion due to syphilis in the area that became known as Broca's area was one of the key finding to suggest localization of function within the brain. The fibres from the cortex on their way to the brainstem pass down in a fan like bundle called the corona radiata to enter the internal capsule. Note that neuroanatomical diagrams are "upside down" compared with the normal appearance of imaging
Histology
Histologically under the microscope the cerebral cortex is made up of a 5mm layer of grey cells above a dense thick inner layer of white matter. The overall surface area is increased by the folds of sulci and gyri. The cortex can be seen to be composed of six layers of cells which vary in size and structure. Back in 1909 Brodmann produced a map of the cerebral cortex based on the micro-architecture of the cells and staining for Nissl substance which separates neurons from glial cells. This was before we had understanding of many of the functions of these areas and the system has stood the test of time. Other improvements have been developed by others. It is quite clear that anatomy is related to function.
Cells in the cortex are arranged in a columnar structure and can this can be seen with microelectrode stimulation. Areas with similar function lie close together. For example Broca's area lies within the inferior region of the precentral motor cortex near to those areas that control voluntary movement of the lips, tongue, larynx and pharynx. Broca's produces the content of speech content and damage here leads to an expressive dysphasia. A lesion in the inferior area of the precentral motor cortex leads to dysarthria and facial weakness. Broca's discovery of dysphasia in a patient whose subsequent post mortem revealed a lesion due to syphilis in the area that became known as Broca's area was one of the key finding to suggest localization of function within the brain. The fibres from the cortex on their way to the brainstem pass down in a fan like bundle called the corona radiata to enter the internal capsule.
Visual Pathway
Embryologically the eye is an outgrowth from the diencephalon. The Optic nerve is formed at the rear pole of the eye exiting medially at the blind spot. It is not a peripheral nerve but a nerve tract and myelinated by oligodendrocytes rather than schwann cells. As such it is not vulnerable to peripheral demyelinating neuropathies but can be affected by central demyelinating diseases eg MS. It leaves the orbit through the optic canal passing medially. At the optic chiasma the nasal retinal fibres cross over and temporal retinal fibres stay on the outside. Fibres cross over at the optic chiasma above the pituitary fossa. The tract passes back send most fibres to the lateral geniculate body as well as ipsilateral pretectal nuclei and superior colliculus. On leaving the lateral geniculate body the tract splits into two tracts with an inferior "Meyer's loop" which passes forwards before radiating posteriorly through the temporal lobe along the inferior horn of the lateral ventricle and then to the lower bank of the calcarine sulcus of the occipital cortex and carries information from the inferior retina. The other fibres loop back more directly through the parietal lobe through the retrolenticular part of the internal capsule before passing on to the occipital lobe particularly the upper bank of the calcarine sulcus.
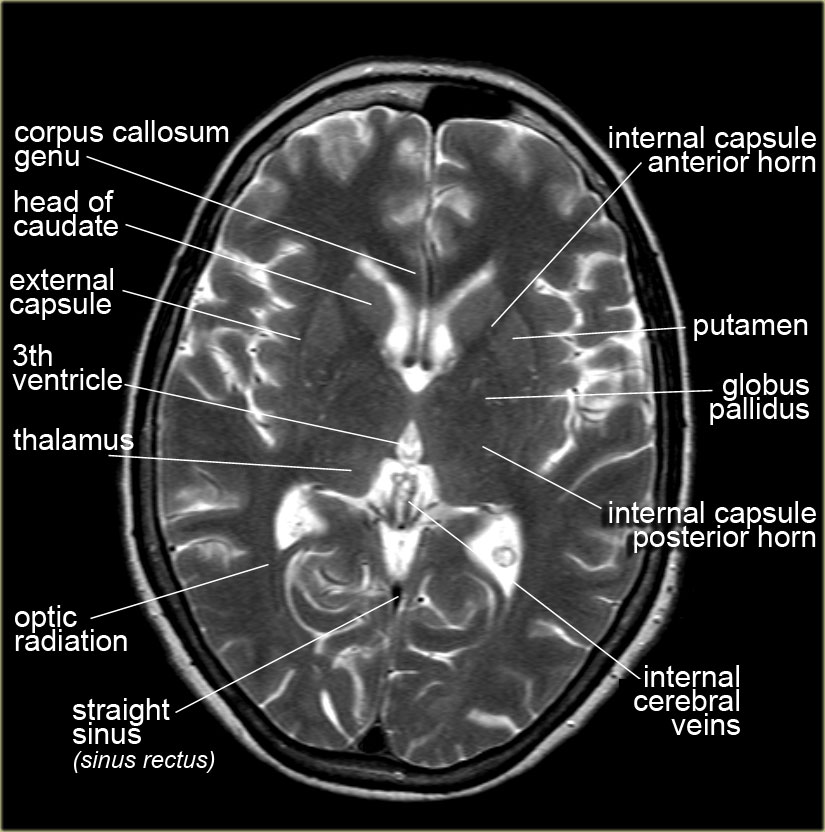
Internal Capsule
This is a right angled shaped tract which carries various both ascending (sensory feedback)and descending (motor) myelinated fibres from the cerebral cortex to the thalamus, brain stem and cerebellum as well as basal ganglia structures. When you see the internal capsule with its almost V like shape on an axial CT or in a simple picture you must appreciate that the axons are running at right angles vertically into the page with information going down (motor) and up (sensory). The fibres come down in a fnalike coronary radiata into the internal capsule. It is sandwiched between the structures of the basal ganglia which is a collection of neuronal cell bodies involved in motor function. It is commonly affected in lacunar strokes. Important ascending (Sensory) and descending (motor/cordination) fibres are densely packed here so small lesions here can cause significant clinical deficits. On a horizontal section or axial view on MRI it can be seen to have an almost half X shape. Fibres that go through the internal capsule then pass into the crus cerebri or Cerebral peduncle. Anatomically it can be said to have four parts.
| Section | Contents |
|---|---|
| Anterior limb | lies between lentiform nucleus ( composed of the Globus Pallidus medially and the Putamen laterally) and head of caudate nucleus medially. It contains ascending thalamocortical and descending corticothalamic fibres connecting lateral thalamic nuclei and the cortex. Fibres from cortex to pons also travel within the anterior limb. Supplied by medial striate branches of the anterior cerebral artery and lateral striate branches of the middle cerebral artery. |
| Genu | This the knee or bend in the L shape which points medially. Contains the corticobulbar fibres which is motor to the cranial nerve nuclei. Supplied by branches of the anterior choroidal artery or direct from internal carotid. |
| Posterior limb | Relations are thalamus medially and lentiform nucleus laterally. Carries the clinically important descending corticospinal tract from the precentral gyrus. Also carries ascending 3rd order sensory fibres from the thalamus to the post central gyrus. Supplied by branches of the anterior choroidal and lenticulostriate arteries. |
| Retrolentiform | Area where it extends past the lentiform nucleus. May contain some visual radiations and auditory fibres. |
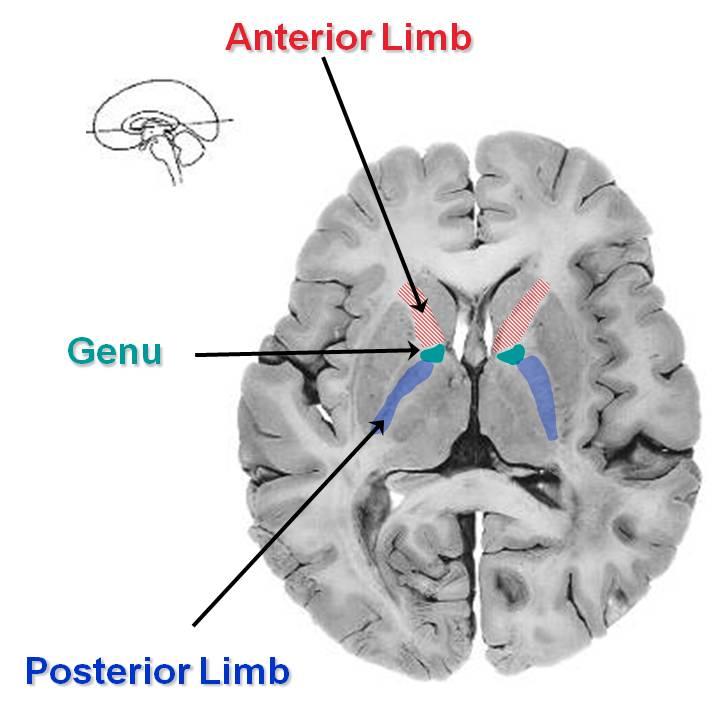
Vascular supply to the internal capsule is by small right angled penetrating arteries of the MCA called the lateral striate (lenticulostriate) arteries and the more anterior aspects including anterior limb by branches of the anterior choroidal artery (a branch of the ICA).
Basal ganglia
The basal ganglia is a collection of interconnected nuclei (neuronal cell bodies) lying deep below the cortex. It is composed of the following structures. The putamen (laterally) and globus pallidus (medially) form the lenticular or lentiform nucleus (lens shaped). The caudate and putamen are also called the neostriatum. Grey matter strands cross the internal capsule to connect these structures and so gives the area the name of the corpus striatum. The putamen is the larger ovoid mass which lies laterally with its lateral side separated very slightly from insular cortex and the external capsule and claustrum. Medially attached to the Globus Pallidus. The Globus Pallidus is smaller triangular shaped structure and lies medially with its medial relation being the internal capsule. The globus pallidus is a major source of output from the basal ganglia. It is divided by a lamina into Globus pallidus externa and interna.
Caudate Nucleus
The caudate nucleus is a large mass of grey cells making up a head, body and tail. Anteriorly seen on scans at the lateral border of the anterior horn of the lateral ventricle. It lies then on the lateral wall of the ventricle and there is a tail which passes to form the roof of the inferior temporal horn of the ventricle. The internal capsule separates it from the putamen. The caudate is notable as being diminished in size in Huntington's chorea. The caudate and putamen receive stimulatory input from the cerebral cortex mediated (Glutamate) and from the substantia nigra (Dopamine). The caudate/putamen gives inhibitory output (GABA) to the Globus pallidus and substantia nigra. The Globus pallidus and Substantia nigra also send inhibitory signals to the ventral thalamic nucleus of the thalamus (GABA) which in turn feeds to the cortex (glutamate). The Basal ganglia is concerned with movements of the contralateral limbs and it would seem that it stimulates and inhibits various regions thus modulating motor output. All of these structures are prone to lacunar infarcts and deep haemorrhage
Subthalamic nuclei
This is part of the basal ganglia. Damage here can lead to dyskinesias and hemiballismus and associated motor disorders.
Diencephalon :Thalamus + Hypothalamus
The thalamus is the largest mass of cell bodies within the nervous system. The thalamus may be affected by both haemorrhage and infarction involving the posterior cerebral artery and its branches. It is a large paired egg shaped structures sitting opposite each other across 3rd ventricle. Contains discrete collections of neuronal cell bodies called nuclei. Separated by a y shaped internal lamina. All but the reticular nucleus send fibres to the cortex. Receives all sensory stimuli (except olfactory) including from the cerebellum, spinal cord and cranial nerves. Bilateral thalamic strokes can cause amnesia as well as hypersomnolesence. Others cause hemisensory loss. Thalamic damage can also lead to so called thalamic pain syndromes where patients experience severe often sharp neuropathic pain in the corresponding contralateral side and it is notoriously hard to treat satisfactorily and causes much morbidity. It contains several discrete thalamic nuclei. The hypothalamus has a minor role to play in stroke so is not mentionned here.
- Medial dorsal thalamus
- Anterior thalamus
- Back of thalamus
- Lateral Geniculate body: Fibres from the optic tracts
- Medial Geniculate body: fibres from inferior colliculus
- lateral thalamus
- Dorsal nucleus
- Ventral nucleus
Brainstem (Rhomboencephalon)
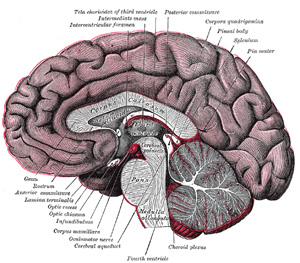
Midbrain
V-shaped structure seen on axial imaging. Contains the following structures.
- Oculomotor nerve nuclei dorsally
- Trochlear nerve nuclei dorsally
- Corticospinal/bulbar tracts ventrally
- Red nucleus
- Substantia nigra
Pons
The Pons has a distinct bulbous appearance on cross section due to large axonal bundles of cell groups which pass through it with descending motor fibres and ascending sensory modalities. There are also groups of fibres running transversely between large pontine nuclei and the two cerebellar hemispheres. Cranial nerves also exit. Laterally lies the bulging middle cerebellar peduncle. The pontine nuclei mediate fibres coming from cerebral cortex to the cerebellum. The VI, VII, VIII and V nerves all leave ventrally. As its name suggests it is bridge like and like any bridge it is a major crossover centre for fibres carrying signals bidirectionally from above and below and communication with the cerebellum. Like any bridge it covers the CSF filled 4th ventricle which separates it from the cerebellum with its vermis and hemispheres which sit tightly behind. It is indeed a bridge over water.
The Pons contains the Corticospinal fibres, Corticopontine fibres, Pontocerebellar fibres and Raphe nuclei. The lower Pons contains the Nucleus of VI, Nuclei of VII, Facial nerve, Superior salivatory Gustatory. The facial nerve and abducent nerve are closely associated as the exiting VII nerve loops around the nucleus of VI. Also contained is the Medial lemniscus (carries contralateral dorsal column), Spinothalamic tract (carries pain and temperature) and Middle cerebellar peduncle which contains fibres from c/L pons to cerebellum.
- Medial
- Medial longitudinal fasciculus
- Medial lemniscus (carries contralateral dorsal column)
- VI (Abducent) nerve nucleus and fibres
- VII (Facial) (fibres closely associated with VI)
- Corticospinal tract
- Laterally
- Facial nucleus VII and nerve fibres
- Spinal nucleus and tracts of V
- Lateral spinothalamic tract (spinal lemniscus)
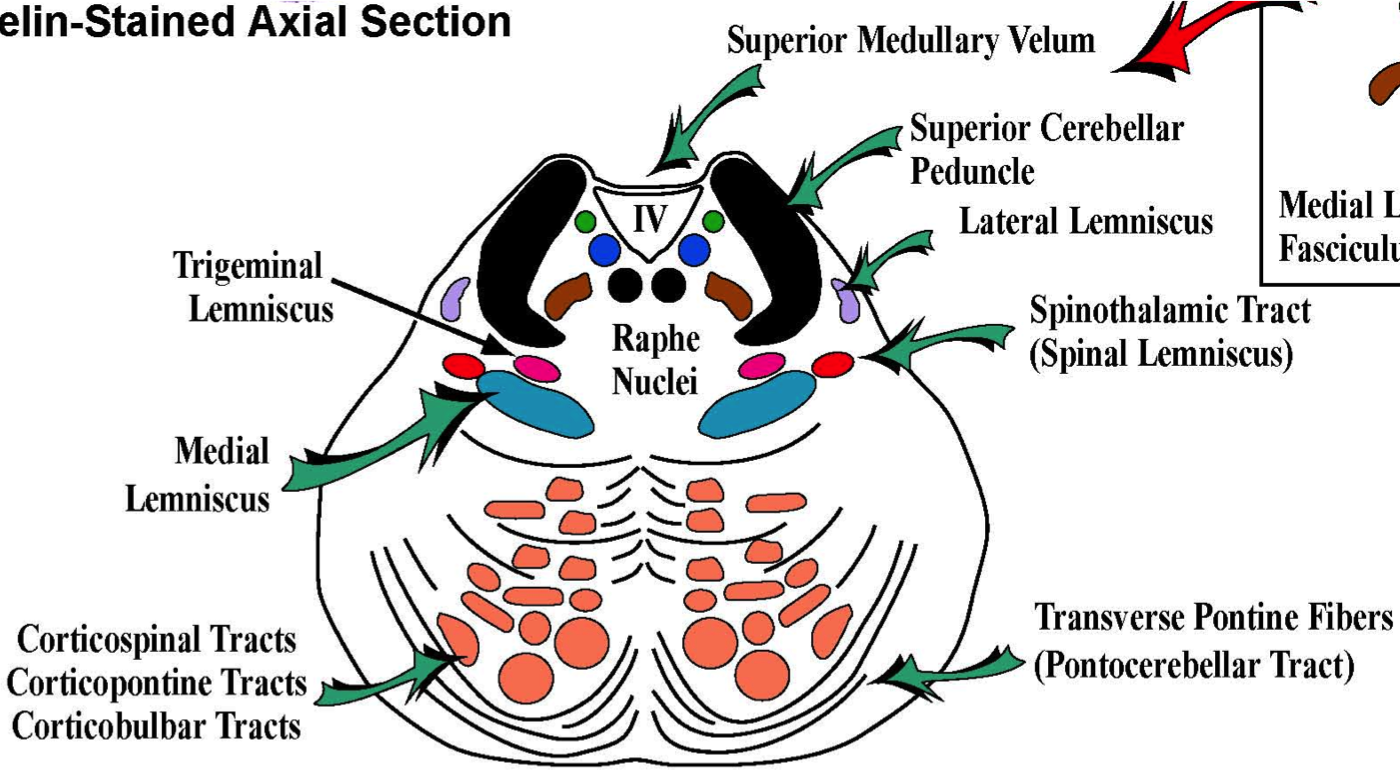
Vascular supply is from the basilar artery which lies anteriorly and provides median and paramedian perforators. Short circumferential branches irrigate more laterally and laterally including the middle cerebral peduncle is supplied by branches of the superior cerebellar and anterior inferior cerebellar arteries.
Medulla
The medulla contains a host of nuclei all tied up with fairly primitive functions such as cardiorespiratory, vomiting centres etc. It also contains the reticular activating system. Medially to the olive and near the midline is the medial lemniscus that carries dorsal column sensation to the thalamus.
- Vascular supply is by branches of the vertebral artery including the posterior inferior cerebellar artery which irrigates the lateral medulla. Lateral medullary syndrome is more commonly due to vertebral occlusion than PICA occlusion of itself.
- Anteriorly there are median and paramedian perforators from the vertebrals.
- Medial
- Hypoglossal nerve nucleus controls tongue muscles.
- Medial lemniscus with crossed fibres from the dorsal column (gracile and cuneate nuclei) on the way to the ipsilateral thalamus
- Pyramids lie on either side of the midline on the ventral surface and contain the corticospinal motor tracts which are decussating.
- Laterally
- Nucleus ambiguus : Efferents to IX and X and XI. Concerned with swallowing.
- Descending nucleus of V: carries pain and temperature from face.
- Dorsal motor nucleus of X : preganglionic parasympathetic to IX and X. Supplies heart, lungs and abdominal organs.
- Nucleus solitarus : Input from VII, IX and X. Partly gustatory nucleus concerned with taste. Fibres pass to venteroposteromedial nucleus of thalamus.
- Inferior olivary nucleus which sends fibres to the cerebellum
- Vestibular nuclei : four of these lie in floor of the IVth ventricle.
- Cochlear nuclei : closely associated with vestibular nuclei
- Inferior cerebellar peduncle with dorsal spinocerebellar, olivocerebellar and cuneocerebellar tracts
- Spinothalamic tract (spinal lemniscus)
- Spinal nucleus of V: Fibres concerned with touch, pain and temperature from the face goes to the spinal nucleus of V. Descend from pons down to the medulla.
- Descending sympathetic fibres
Cranial nerves
| Cranial nerve | Nucleus | Actions | |
|---|---|---|---|
| 1. | Olfactory | Olfactory bulb | Smell to the temporal lobe carried in the olfactory bulb |
| 2. | Optic nerve | Lateral geniculate nucleus | Retinal output to the optic chiasm. |
| 3. | Oculomotor nerve | Upper Midbrain |
|
| 4. | Trochlear nerve | Lower Midbrain |
|
| 5. | Trigeminal nerve | Pons |
|
| 6. | Aducens nerve | Pons |
|
| 7. | Facial nerve | Pons |
|
| 8. | Vestibulocochlear nerve | Pons |
|
| 9. | Glossopharyngeal nerve | Medulla |
|
| 10. | Vagus nerve | Medulla |
|
| 11. | Spinal accessory nerve | Medulla |
|
| 12. | Hypoglossal nerve | Medulla |
|
Cerebellum
The cerebellum contains as many neurons as the entire cerebrum. Its primary role is the coordinating motor function with other parts of the brain. It is composed of a core of white matter surrounded by grey matter. The cerebellum also consists of a cortex covered in grey matter folded into folia with deep fissures. Anatomically it is closely related to the IVth ventricle and contains 4 deep nuclei called the dentate, emboliform, globose and fastigial. The cerebellum receives sensory input as well as input from the motor and premotor cortex and returns feedback to these same centres. As such the cerebellar hemispheres deal with ipsilateral movement and function. Cerebellar hemispheres communicate via inferior, middle and superior cerebellar peduncles. Inferiorly lie the cerebellar tonsils which are important in Arnold-Chiari malformations. The cerebellum is separated from the pons by the fourth ventricle. Histologically the important functional cell is the Purkinje cell which lies between the molecular and deep granular layer of cells. The purkinje cells communicate with the deep cerebellar nuclei (dentate, emboliform, globose and fastigial (Easily remembered as DEFG)) . They usually project inhibitory output using GABA to cerebellar and vestibular nuclei.
The cerebellum is composed of a midline vermis and two lateral cerebellar hemispheres. It is composed of anterior and posterior lobes and flocculonodular lobe. The vermis is concerned with midline and truncal position and receives input from the spinal cord. Dysfunction is noted by postural instability and gait ataxia. Processing occurs in the cerebellar hemisphere and output is via the superior cerebellar peduncle which decussates in the midbrain and whose fibres pass to the motor nuclei of the thalamus and from there back to the motor and premotor cortex.
Cerebellar peduncles
The cerebellum attaches to the posterior aspect of the brainstem by 3 large tracts, the superior, middle and inferior cerebellar peduncles. Do not confuse these with the cerebral peduncle.
- Superior cerebellar peduncle: (brachium conjunctivum) contains efferent fibres from the cerebellum that pass superiorly and includes the major outlow tract from teh cerebellum which is the dentatothalamic tract. This passes to the ventral lateral nculeus of the thalamus. It also receives the ventral spinocerebellar tract from the spine.
- Middle cerebellar peduncle (brachium pontis) attaches to the pons. It has afferent fibres from the pons - the pontocerebellar fibres. The cerebellar hemispheres receive input from the contralateral motor and premotor cortices by fibres which have decussated in the pons and enter the cerebellum via the middle cerebellar peduncle. The middle peduncle brings input from pontine nuclei.
- Inferior cerebellar peduncle attaches to the medulla and receives input from the spinal cord. Receives the dorsal spinocerebellar fibres, the cuneocerebellar tract and the olivocerebellar tract from the contralateral inferior olivary nucleus
Cerebrospinal fluid
CSF is formed from the choroid plexuses in the lateral (70%), third (5%) and fourth (5%) ventricles and ependymal cells(20%) lining the ventricles. The epithelium of the choroid plexus forms a barrier between blood and CSF filtering out various substances. CSF Flow is from the lateral ventricles through the foramen of Munro into the third ventricle and then through the aqueduct of Sylvius into the fourth ventricle. The aqueduct is only 2 mm in diameter and is a common site of CSF flow blockage. From there it drains through one of three foramina either laterally through the foramina of luschka (lateral) or the medially placed foramen of Magendie. CSF then enters the subarachnoid space. It is finally absorbed by the arachnoid villi into the venous sinuses. Obstruction at the level of the aqueduct causes a non communicating hydrocephalus. Obstruction to CSF flow at the level of the arachnoid villi causes a communicating hydrocephalus. Lumbar puncture is not contraindicated, in fact it may be diagnostic as well as therapeutic in those with a communicating hydrocephalus where pressures are freely transmitted through the subarachnoid space. CSF is produced by the action of the Na+/K+ ATPase pump actively moving Na+ ions into the lumen of the ventricles which is then followed by h40. This happens in the cuboidal cell epithelial cells that form the choroid plexus. The choroid plexus releases about 500 mls of CSF per day into a volume of 100-150 ml. The choroid plexus selectively filters the CSF so that its content differs from plasma. CSF has a lower glucose, very much lower protein, low urea and a low amino acids content. CSF protein is 1/1000th that of CSF. CSF means that the brain basically floats such that the effective weight of the brain is reduced from 1400 g to about 50 g. The CSF also plays a role in the continual drainage of the ventricular cavities and subarachnoid space. The CSF is replaced three times per day and enough is produced in 3 days to fill the entire brain free skull volume. It is no surprise that acute hydrocephalus can be an acutely fatal event if unrecognised and untreated.
Membranes
The brain itself is surrounded by 3 membranes sandwiched between it and the skull periosteum.
- BRAIN PARENCHYMA
- Pia: The most closely adherent and inner layer is the pia which is closely related to the surface of the brain sulci and gyri. It is very delicate and vascular covering the brain and spinal cord.
- Subarachnoid space: Blood vessels lie in this plane and it is the plane of bleeding for berry aneurysms. Terminates at S2 in sacral vertebra
- Arachnoid: It is separated from the arachnoid by the subarachnoid space. It is delicate but non vascular.
- Subdural space: traversed by bridging veins which can bleed. Potential space in the spinal cord.
- Dura: Above this lies the dura mater. Between the arachnoid and dura mater is the subdural space where bleeds due to the shearing of veins may be seen.
- Extra (Epi)dural space: between the skull and dura lies the extradural space. Contains meningeal arteries and veins. The dura matter is adherent to the skull at areas where bones fuse which limits the spread of blood with extradural haemorrhage. Convex shaped bleeds on CT. In the cord injection of this space may be used to cause anaesthesia.
- SKULL PERIOSTEUM
Fibrous Membranes
- Falx cerebri which is a vertical membrane that separates right and left cerebral hemispheres. If there is a rapidly expanding unilateral cerebral space occupying lesion or extra-axial lesion (EDH or SDH) can force the uncus of the temporal lobe under the falx.
- Falx cerebelli separate the right and left lobes of the cerebellum.
- Tentorium cerebelli lies between occipital cortex and superior surface of cerebellae. This helps enclose the cerebellum within the bony and membrane bound posterior fossa where for example a large cerebellar haematoma needs evacuation before it can cause an acute rise in pressure compressing the brainstem or causing hydrocephalus.
Next: >> Stroke Neuropathology |
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |