Learning objectives
- What is moyamoya disease
- Clinical presentation
- Useful tests
- Managment of moyamoya disease
|
Introduction
- This is a progressive non inflammatory vaso-occlusive disease
- There is bilateral stenoocclusive changes at the terminal portion of the ICA
- There is an abnormal vascular network formation at the base of the brain.
- It is a cause of both ischaemic and to a lesser extent haemorrhagic stroke.
- It can be inherited or acquired. It may present in childhood.
- Japanese described it in 1957 as “hypoplasia of the bilateral internal carotid arteries” [1]
- Later characterised as "moyamoya" in 1965.
- Commonest in Asian (Japanese, Chinese and Koreans) it does occur in other non Asian populations.
Epidemiology
- It is seen in up to 10 per 1000,000 in Japan but in the USA the incidence falls to less than 1 in 1,000,000
- Not exclusive to non asian populations
- Bimodal onset age 10-14 years and smaller peak in the 40's
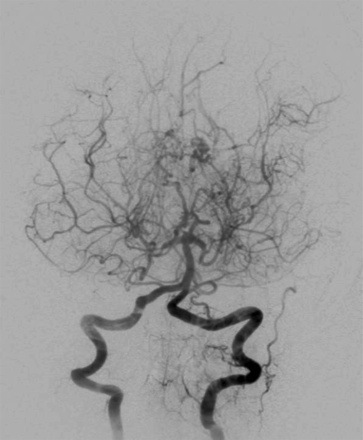
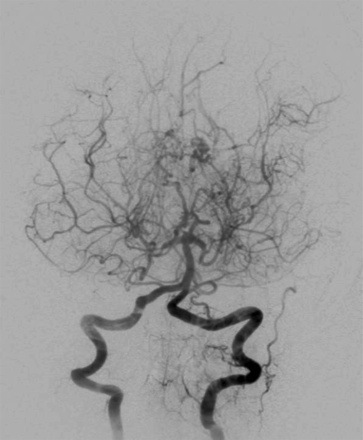
| The abnormal netÂlike vessels at the base of the brain seen in cerebral angiograms of this disease were described by most native speakers of Japanese as "moyamoya," a Japanese expression for some thing hazy, such as a puff of cigarette smoke drifting in the air. The name was popularised by Jiro Suzuki. [Suzuki J et al. 1983]
|
Aetiology
- Familial cases are linked to a gene on Chromosome 17.
- Cases are both sporadic and familial.
- Overexpression of angiogenic and endothelial growth factors.
- Increased levels of Basic fibroblast growth factor has been found in MMD which is one of several areas of further research.
Causes of Moyamoya Syndrome
- Sickle cell disease, Beta thalassaemia,
- Neurofibromatosis type I
- Fanconi anaemia
- Hereditary spherocytosis
- Homocystinuria and hyperhomocysteinemia
- Takayasu's arteritis
- Fibromuscular dysplasia
- Factor XII deficiency and Essential thrombocythaemia
- SLE, Grave's Disease, APS and various other genetic disorders.
Pathophysiology
- There is progressive intracranial artery stenosis and occlusion of the internal carotid artery
- Formation of fragile collateralisation arteries which can bleed.
- Major artery and peripheral artery aneurysms can also be found.
- Bleeding is seen more so in adults and is the main cause of mortality and morbidity.
- Bleeding is both from fragile collaterals and rupture of saccular aneurysms on the circle of willis or from dilated perforators [Kuroda S 2008].
- Most commonly Children present typically with recurrent episodes of sudden hemiplegia that might alternate sides.
- Moyamoya disease can affect children and young people with TIA episodes.
- May also be strokes, chorea and seizures.
- It causes predominately ischaemic stroke but haemorrhagic stroke is also seen due to bleeding from fine collaterals and is commoner in Adults.
Classification
| The Angiographic stages Modified from Suzuki [Suzuki 1969] by Burke [Burke et al. 2009] |
|---|
| Stage | Description |
|---|
| 1 | Stenosis of the suprasellar ICA usually bilateral |
| 2 | Development of Moyamoya vessels with dilatation of all main cerebral arteries at base of brain |
| 3 | Increasing ICA stenosis and prominence of Moyamoya vessels with reduction of flow in the MCA and ACA |
| 4 | Entire Circle of Willis and PCAs occluded. Extracranial collateralisation with minimisation of Moyamoya vessels. Proximal portions of the PCA become involved |
| 5 | Reduction of Moyamoya and absence of all main cerebral arteries |
| 6 | Disappearance of Moyamoya vessels and major cerebral vessels; the cerebral circulation is supplied only by the external carotid system |
Investigations
- Bloods: unremarkable usually (non inflammatory vasculopathy)
- CT Imaging can show either cortical or subcortical infarction and even some cortical volume loss. Subcortical lesions seem to occur earlier. CT can also show deep and lobar haemorrhage.
- MRI/MRA should be performed for the diagnosis. This shows carotid narrowing or occlusion in the distal internal carotid and fragile collateral vessels give traditional "puff of smoke" appearance on cerebral angiography.
- MRI Gradient echo may show prior or new haemorrhage. The finding of dilated collateral vessels in the basal ganglia and thalamus can be demonstrated as multiple punctate flow voids and is regarded as virtually diagnostic of Moyamoya syndrome.
- MRI FLAIR images and post contrast T1 images can show a linear pattern of increased signal in the leptomeninges and perivascular spaces. This pattern has been termed the "ivy sign", since it resembles the appearance of ivy creeping on stones.
- Transcranial Doppler ultrasonography if available is a noninvasive way to evaluate intracranial haemodynamics and large artery stenosis.
- EEG: Moyamoya syndrome-specific alterations of EEG recordings are only observed in children. These consist of a gradual frequency decrease and amplitude activation after hyperventilation. This is referred to as re-build-up phenomenon. Thus, a tentative diagnosis of Moyamoya syndrome in children can be based on the EEG finding. This should be radiologically confirmed by angiography. [3]
- Perfusion studies: may show up areas of brain at risk of ischaemia and infarction [4]
Management
- Management includes medical and surgical options. Patients are referred to centres of excellence with experience in this disease.
- Medical options are unproven but include vasodilators and some would avoid antiplatelets especially in older patients.
- General blood pressure management would seem wise. Most would consider surgery in symptomatic patients.
- There are a variety of procedures to increase blood supply.
- Surgical treatments are divided into 3 types: direct, indirect, and combined/other methods. Direct bypass includes superficial temporal artery (STA) or sometimes the occipital artery to Middle cerebral artery (MCA) anastomosis or use of other graft types. Indirect procedures bring in circulation to the intracranial regions by introducing newly developed vasculature from newly approximated tissues. Recent evidence tends to favour a direct strategy in reducing haemorrhagic risk.
- Multiple burr holes can aid revascularisation [5]
- Children are given aspirin but without any real evidence base and it is stopped in adults due to risk of bleeds.
- Haemorrhagic lesions are the commonest cause of death.
Further Reading
|
|
Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site.
|