Introduction
The overriding concept in hyperacute care is that "time is brain" and that systems must be in place to rapidly receive acute stroke patients and quickly assess them. There are two real streams, those who may be suitable for urgent and active therapies and others who need general physiolgical support and the prevention of complications. Urgent therapies would include Stroke Thrombolysis and Mechanical Thrombectomy and reversal of anticoagulation to halt haemorrhage in those with ICH such as those on anticoagulants and those deteriorating due to massive ischaemic or haemorrhagic stroke due to oedema or hydrocephalus or haematoma who may benefit from decompression, External ventricular drainage (EVD) or craniectomy. These patients will become immediately apparent.
Hospital care
The key is to have stroke trained staff receiving these patients with no needless delays holding up the process. Once seen, immediate CT scanning should be done and this will aid management. Locally we aim to deliver thrombolysis within 20 minutes from arrival so we meet and greet the patient, get a handover from paramedics, establish time of onset and any possible contraindications to lysis such as anticoagulation. In the meantime, the patient is quickly booked on systems and CT head booked and it's straight off to CT taking a history and examining on the way and while waiting. The history is focused as is the examination. Family are kept close by to help information gathering and they may be involved in the consenting process. The doctor and stroke nurse push the patient to CT and help radiology staff and at no point should the patient be waiting with no productive activity in place. One the CT is done it can be inspected, the BP re-checked, the weight verified, and a quick checklist of contraindications and consent checked then we can prescribe and administer Alteplase. There is no need to do an ECG or to await blood results on the majority of patients. Each hospital has its own distinct preferences, some thrombolyse in the emergency department, others on the Hyperacute stroke unit. The main issue is to continually review your pathway to make sure it is efficient and safe and remove needless delays. Small improvements can all add up to significant reductions in door to needle times. The initial stroke cased is based around several basic principles of identifying early acute interventions which may help and protecting the patient from complications.
| Actions | Comments |
|---|
| ABC | Urgent management of airway, ventilation, and circulation is vital in patients who have decreased levels of consciousness. Supplemental oxygen is not recommended in nonhypoxic patients. If GCS < 9 assess for ITU bed. Intubation for those who cannot protect airway and ventilate those not breathing. End of life care may be more appropriate in catastophic stroke. Assess NIHSS |
| Blood glucose | Treat and manage any hypoglycaemia by fingerstick blood draw is acceptable |
| Assess those with Ischaemic stroke for Stroke Thrombolysis | Consider for Stroke Thrombolysis and administer recombinant tissue plasminogen activator within 3 hours (age >80) or 4.5 hrs if Age (<=80) of symptom onset, after appropriate screening for ischaemic stroke. Non contrast CT scan. Determine eligibility for thrombolytic therapy. Ensure door to needle time < 30 mins. Avoid in Patients with known or suspected bleeding diathesis or anticoagulant use: review coagulation studies and platelet count to ascertain eligibility before proceeding |
| Assess those with Ischaemic stroke for Thrombectomy | If anticipating Mechanical Thrombectomy then get an urgent CTA to look for large vessel obstruction as early as possible but within 6 hours; may be considered in select patients for window of up to 16 to 24 hours with the aim being reperfusion to a modified thrombolysis in cerebral infarction 2b/3 angiographic result to maximize the probability of a good functional clinical outcome |
| Haemorrhagic stroke or Ischaemic stroke and raised ICP | Discuss need for neurosurgical intervention as appropriate. May need Shunting for those with hydrocephalus or Sub-occipital craniectomy for cerebellar bleeds or Neurosurgical referral for Clot evacuation or Decompressive Hemicraniectomy for malignant MCA syndrome or Coiling or clipping for those with SAH |
| Haemorrhagic stroke and coagulopathy | 4 factor Prothrombin complex concentrates and Vitamin K for Warfarin or DOAC induced bleeds. Praxbind for Dabigatran. Platelets for thrombocytopenia |
Key facts to acquire before referral to thrombolysis/thrombectomy
| Actions | Comments |
|---|
| Age of patient | Defines thrombolysis window. Aged < 80 we treat up to 4.5 hrs and over 80 only 3 hrs |
| Time since last well | Time of onset is very useful but if this is unclear we must use Time since last well and time found and work out when we think time of onset was to some degree of accuracy if possible to help define the window |
| Anticoagulation | Being anticoagulated contraindicates thrombolysis but not thrombectomy |
| NIHSS | Tells us severity of stroke. We don't usually offer reperfusion therapies on those with small (NIHSS<4) or very large (>25) strokes |
| Premorbid state | Thrombolysis/thrombectomy reduce dependency. If already dependent then benefits less. |
| CT report | We will look at it but do not refer for reperfusion (thrombolysis/thrombectomy) if haemorrhage or tumour or advanced stroke changes suggesting stroke is older than thought. If unsure discuss. |
| Comorbidities | If the patient has advanced malignancy or other diseases possibly contraindicating alteplase. Any recent bleeding issues or trauma must be noted and any non investigated severe anaemia. |
| Blood pressure | Need BP < 185/110 mmHg to give alteplase. |
Managing and Preventing Early complications
| Managing and Preventing Early complications |
|---|
| Bedside Swallow assessment | Checking safe swallow before oral intake reduces aspiration |
| Feeding | NG tube placement for feeding when appropriate |
| VTE prevention | Using methods to prevent VTE - Intermittent pneumatic calf compression, LMWH, Early mobilisation |
| Hydrate | IV fluids to prevent dehydration in those unable to drink |
| Skin care | Regular turns and monitoring to prevent skin damage and ulcers |
| Bowels | Bowel management to prevent constipation |
| Shoulder | Prevention of shoulder damage and postural problems |
| Therapy | Early rehabilitation to enable recovery |
| Seizures | Management of seizures |
| Infections | Management of infections - UTI, RTI |
| Bladder | Management of continence, avoidance of catheterisation where possible |
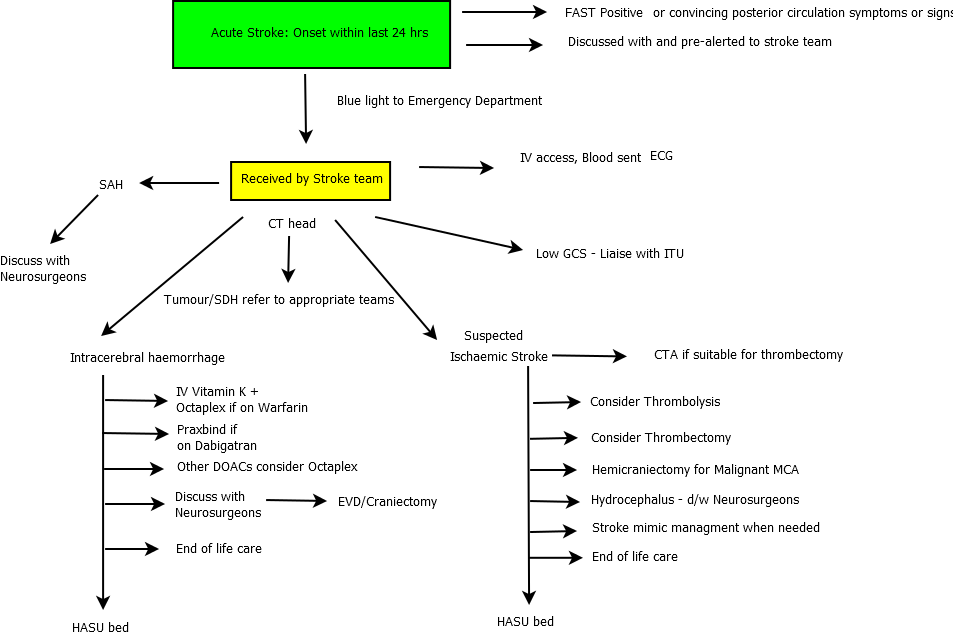
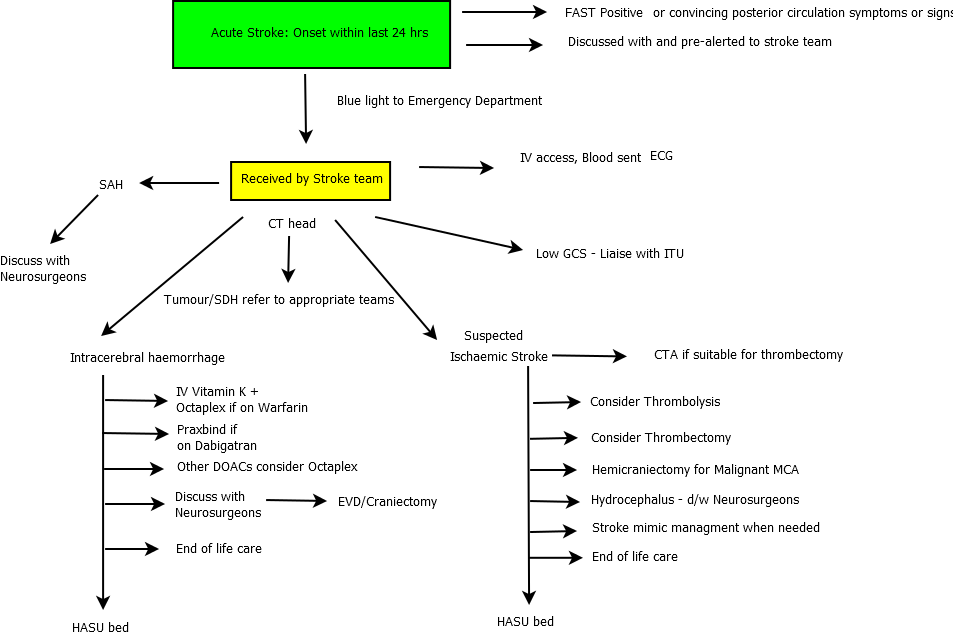
Schematic of a pathway
Last updated: 25/11/2018
|
|
Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site.
|