Learning objectives
|
Introduction
- Carotid dissection (CD) accounts for only 1-2% of all ischaemic strokes.
- In young individuals and middle-aged adults it accounts for 10-25% of these event
- Carotid or vertebral dissection without evidence or suspicion of SAH is not a contraindication to thrombolysis.
- Always ask about unusual neck position or turning or trauma in young strokes
Aetiology
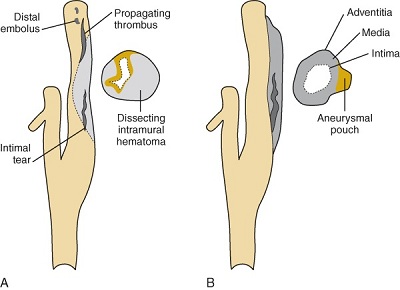
- Dissection occurs when there is a tear in the intimal layer of a blood vessel with bleeding and haematoma formation within the vessel wall.
- The haematoma may be due to an intimal tear and entry of luminal blood or from vasa vasorum or both.
- This can lead to overlying thrombus or vessel stenosis or occlusion.
- The clot can cause complete or subtotal occlusion of the carotid artery or vertebral.
- Damage to the endothelium means that the vessel loses its natural "non-stick-surface" and so clot can form on the luminal intimal surface and cause artery to artery embolisation which is the rationale for anticoagulation/antithrombotic therapy.
- There is a small risk that dissections can extend proximally, and as intracranial vessels are more fragile with a risk of SAH.
- This may temper any desire to anticoagulate and as all of this is an evidence light area, so different clinicians may have different ways to manage these perceived risks.
Epidemiology
- Always consider this diagnosis in a young adult (under 50) with an anterior circulation stroke unless alternative cause is evident.
- The prognosis is felt to be good with a very low rate of recurrence.
- Dissection may be precipitated by any accidental neck trauma or cervical manipulation.
- Carotid dissection is about 3 times commoner than vertebral. Commonest in those in their mid 40s but seen at any age.
- This most commonly occurs in the internal carotid artery approximately 2-3 cm after the bifurcation.
- A very small minority (2%) associated with Marfan's syndrome, Ehlers Danlos Type IV or Fibromuscular dysplasia
- Males and females are equally affected.
 |  |
Clinical
| Presentations of Carotid Dissection |
|---|
|
| Causes of Dissection seen recently | |||
|---|---|---|---|
 |
 |
 |
 |
| A sneeze or other violent neck movement. | Sports such as cricket and rowing. | Blow to the head causing torsional forces - hit with a football. | Following a road traffic accident. |
| Some possible associations with dissection |
|---|
|
| The issue with chiropracter manipulation is that it may be done to ease neck pain which may have been due to a dissection. It may just be association rather than causation for some. |
 | 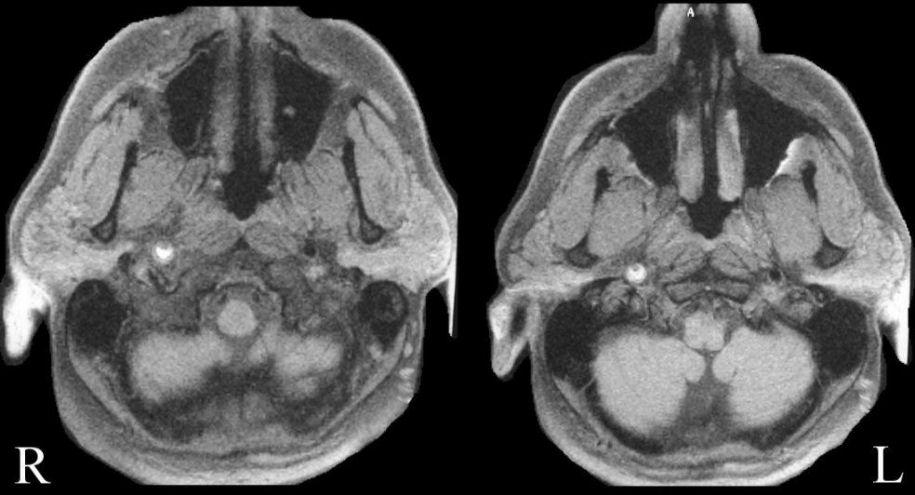 |
| Left Carotid Dissection | Right Carotid Dissection |
Imaging
- CTA or MRA are the preferred noninvasive diagnostic imaging tests for patients with a suspected cervicocephalic artery dissection, as neck ultrasound does not fully visualize the vertebral arteries and can miss distal or carotid dissection originating above the angle of the jaw
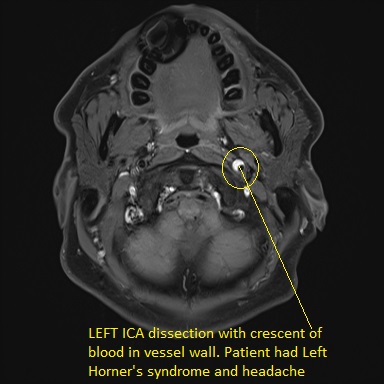
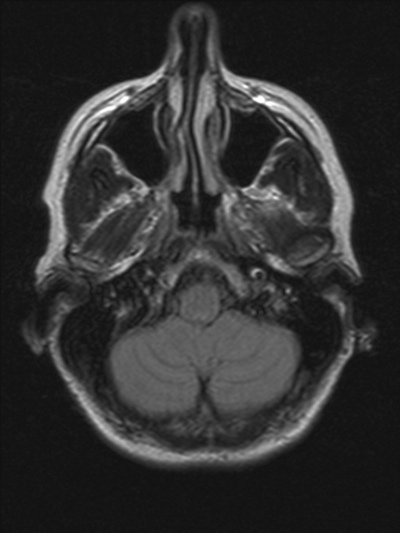
- T1 fat-suppression technique (wall haematoma): crescentic flap within the left internal carotid artery can be seen on MRI T1 with fat suppression/saturation. This crescent-shaped rim of hyperintense signal adjacent can be matched with a narrowed segment of artery on angiography. Infarction if it occurs is either embolic or due to complete occlusion of the vessel. There is a more tapered appearance than seen with an embolic or in situ blockage.
- MRA/CTA/DSA shows obstruction or tapering of the artery
- MRI/DWI may show embolic stroke within the distribution of the affected artery
Management
- ABC and acute thrombolysis/thrombectomy is indicated. Vessel rupture is very rare indeed and dissection is not a bar to reperfusion therapies.
- The main therapy is anticoagulation/antithrombotic therapy to reduce risk of thrombus formation and embolism and to maintain vessel patency. In those with dissection but no stroke or TIA the main risk seems to be in the subsequent 2 weeks but even then risk is low [3]. There is a lack of evidence regarding the use of anticoagulation in intracranial arterial dissection
- The choice has been between Aspirin, clopidogrel and warfarin or even a DOAC. Many would nowadays opt for the ease of using an antiplatelet agent for at least 6 months. The CADISS trial showed no appreciable benefit with warfarin treatment. Choice of therapy depends on whether dissection has been accompanied by a stroke, the size of stroke and risks of haemorrhagic transformation.
- If the patient presents with an acute stroke then thrombolysis should certainly be considered and carotid dissection with out suspicions of SAH is not a contraindication.
- Risk of recurrence seems low especially if the provoking mechanism is avoided. [Debette S. 2009].
Further reading and references
- [1]Dissection of the internal carotid artery causing transient ischaemic attack and Horner's syndrome.J R Coll Physicians Edinb 2009; 39:121-4
- [2]Carotid and vertebral artery dissections . Arnold M, Bousser†MG. Practical Neurology, 2005, 5, 100-109
- [3]Nicholas A. Morris et al. Timing of Incident Stroke Risk After Cervical Artery Dissection Presenting Without Ischaemia
Last updated: 14/11/2018
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |