Learning objectives
|
Introduction
- This is an underdiagnosed syndrome which may mimic SAH
- It is between 2 and 10 times commoner in females. Mean age of onset is 45.
- Can cause Convexity SAH and ICH or Ischaemic stroke in 5-10% [Ducros A et al. 2009].
- The prognosis appears to be excellent for most.
- Also known as Call-Fleming syndrome and postpartum angiopathy
Possible Triggers of RCVS
| Possible Triggers |
|---|
|
| Fisher first described the phenomenon of reversible segmental cerebral vasoconstriction in the early 1970s, in a paper reporting cases of postpartum women with transient neurologic dysfunction associated with reversible cerebral arterial irregularities and the entity became known as "postpartum angiopathy" |
Clinical
- Classically middle-aged female but happens in males too. Older ages too.
- Often severe sometimes bilateral and even daily recurring headaches often thunderclap
- There may be associated nausea and sickness but not to the degree of migraine.
- May also cause seizures and focal neurological deficits.
- The headache which is the dominant feature may wane after 1-3 hours leaving behind a 'background' headache.
- The headaches can persist almost daily for several weeks.
| Criteria for RCVS [Calabrese et al. 2007] |
|---|
| Acute and severe headache (often thunderclap headache) with or without focal neurological deficits or seizures |
| Monophasic course without new symptoms more than 1 month after clinical onset |
| Segmental vasoconstriction of cerebral arteries demonstrated by angiography (MRA, CTA or catheter) |
| Exclusion of subarachnoid haemorrhage due to a ruptured aneurysm |
| Normal or near normal CSF (protein <1g/l, white cells < 15/mm3, normal glucose) |
| Complete or marked normalisation of arteries demonstrated by a repeat angiogram (MRA, CTA or catheter) after 12 weeks, although they may be normal earlier |
Differentials of Thunderclap headache and stroke
- Subarachnoid haemorrhage
- Primary Angiitis of the Central Nervous System
- Cervical dissection
- Cerebral venous Thrombosis
- Migraine
Investigations
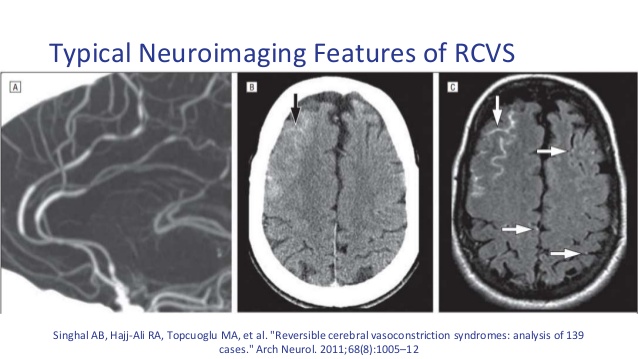
- CT head: usually normal but may show subarachnoid blood over sulcal convexities
- CTA: May show spasm of branches of the COW which resolves on later scanning at 12 weeks
- LP result - see table on previous page
- MRI T1/T2/FLAIR/GRE/DWI/ADC/MRA/MRV and Cervical T1 with fat saturation and contrast. MRI will show infarction or bleed. It may show changes of posterior reversible encephalopathy (symmetrical high signal on FLAIR) or Subarachnoid or subdural bleeding.
- DSA: is superior to MRA/CTA and shows various segmental narrowing 'string of beads' of the intracranial vessels which disappear on angiograms within 12 weeks. Vasoconstriction may be missed if angiography done too early. Vasoconstriction may not peak for several weeks after presentation. The CSF which should be done to exclude SAH is usually normal but of there is even small rise in lymphocytes it is prudent to repeat a few weeks later to demonstrate normality and exclude chronic meningitis.
- Transcranial Doppler may be used to monitoring the cerebral vasoconstriction producing increased flow velocities. RCVS may be mistaken for Primary Angiitis of the Central Nervous System (PACNS) due to the presence of similar angiographic features of segmental narrowing of cerebral arteries.
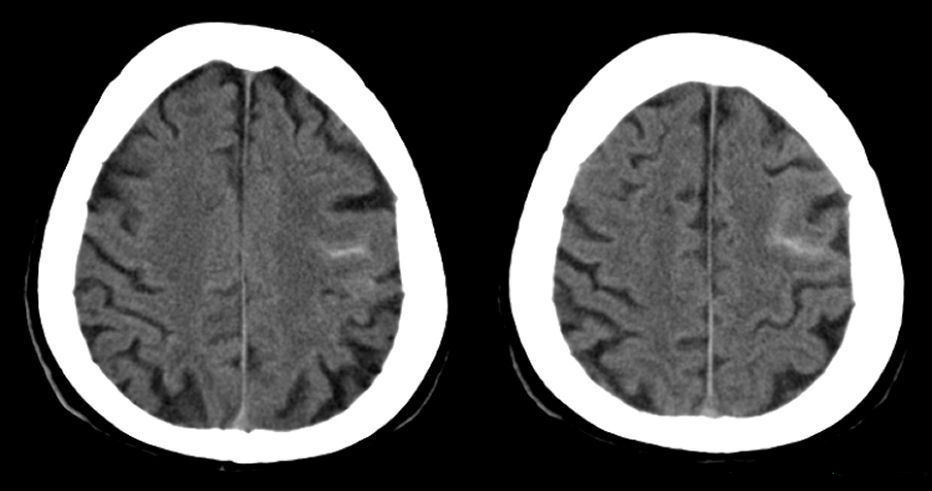
| Note the subtle sulcal blood which can be very easy to miss. This can cause focal seizure and weakness and is a stroke mimic. I have seen subtle bleeding like this missed by experts and patient thrombolysed with disastrous outcome. |
Management
- ABC, Hydration acutely and exclude SAH if needed. May need a CTA/MRA/DSA to exclude aSAH.
- Calcium channel blockers such as Nimodipine or Verapamil have been used. Other agents are under investigation.
- Despite stroke risk 95% of patients have no long term neurological deficits in two large prospective series [Chen et al. 2009; Ducros et al. 2007].
References and further reading
- Ducros A et al. Reversible cerebral vasoconstriction syndrome Lancet Neurol 2012; 11: 906-17
- Calabrese et al. Narrative Review: Reversible Cerebral Vasoconstriction Syndromes Ann Intern Med. 2007;146(1):34-44.
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |